Elizabeth Hughes Gossett shouldn’t have survived beyond 11, the age at which she developed type 1 diabetes. Born in Albany, New York, Gossett received her diagnosis in 1918 when diabetes had no known treatment. Tragically, her life expectancy was just a matter of months. Her parents desperately searched for any way to keep their daughter alive. A New Jersey physician had developed a radical course of action: keeping the blood sugar levels of diabetic children low by feeding them the bare minimum needed to survive. This could see a prognosis of months extended to years. These young patients weren’t exactly living, but they were alive.
In the spring of 1919, Gossett went into this starvation clinic. She’d have been constantly cold and hungry. Emaciated, unable to move or grow. At its lowest, her weight dropped to 20kg. Three years later, Gossett was lingering on death’s threshold but, crucially, hadn’t crossed to the other side.
“And as result,” Dr Ariel Zeleznikow-Johnston explains to me, “she was still alive when, in 1921, what had hitherto seemed impossible was achieved: insulin treatment was developed.” Gossett received her first injection of the hormone in 1922 and started to eat again, move again, live again. She survived into her 70s, taking about 42,000 insulin shots in that time.
“You see,” Zeleznikow-Johnston says, “for millions of years, people just died from diabetes, something that was thought to be inevitable. Unchangeable. Then suddenly, from nowhere, this was no longer true.” In Gossett’s case, there was a limbo period: years between her diagnosis and a treatment becoming available. “In 1918, most kids diagnosed with type 1 diabetes died. Elizabeth didn’t, because the pause button was pressed and, as a result, a future was bought for her. That’s what I’m advocating for.”
It’s this idea which lies at the heart of Zeleznikow-Johnston’s new book, The Future Loves You: How and Why We Should Abolish Death. A manifesto for – and road map to, he hopes – today’s terminally diseased and dying being offered a pause button of their own. A chance to halt their biological clocks, until such a time that science and medicine has advanced sufficiently. Maybe, even, the prospect of immortality. He’s convinced the technology already exists to make much of this possible, and costs little more than a midrange secondhand car.
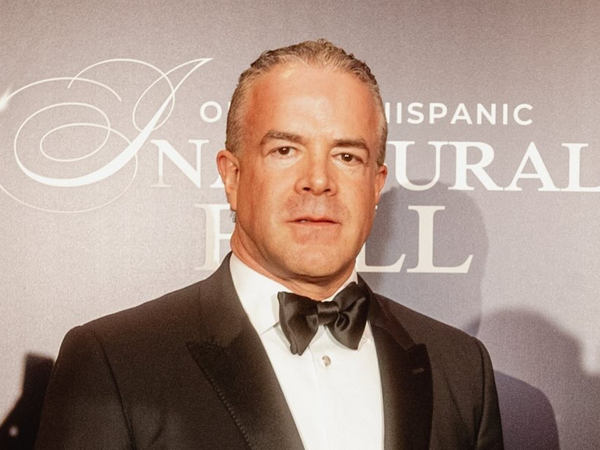
Zeleznikow-Johnston, 31, is a research fellow at Melbourne’s Monash University. “I’ve been interested in neuroscience forever,” he says, from his recently acquired, bright, campus office. “It’s the confluence of biology – the wet mechanics – of how cells and neurons work, philosophical questions of identity, and the fun, cognitive mechanics of how the brain functions.” You know that feeling of having a word on the tip of your tongue, but can’t quite get it? “Working out what’s happening there,” he says, “is basically my day job. Exploring how brains give rise to consciousness.”
He’s also interested in the history of medical progress and where the future lies. “Logically, where we can expect this technology to be in 10, 20, 100 years from now. That’s what took me to the prospect of preservation: how we might still be around in decades and centuries to come.” In other words, could we give ourselves a shot at making use of medicine’s far-off advances? “With the advent of brain preservation,” he writes, “I don’t think that you, or anyone you love, has to die at all.”
First, though, a much simpler question: would you even want life eternal? So outlandish is the notion, you’ve likely given it little thought. In his line of work, it’s a topic Zeleznikow-Johnston finds himself grappling with regularly. “Reminders that my brain and body are constantly decaying,” he says, “can become a bit much from time to time; it can feel heightened. And I’ve always been suspicious that our societal acceptance of death comes from an inability to imagine anything otherwise.” It’s a hunch, he says, that’s not purely anecdotal: scientific literature, he mentions, backs him up.
“Studies show that if you survey people across all ages,” he says, “and ask how long they’d like to live for, most only ask for five to 10 years longer than their demographic is statistically likely to get: 90, let’s say.” Zeleznikow-Johnston believes this presents an incomplete picture.
Research also shows these answers change when it’s stipulated that respondents would be guaranteed good mental and physical health into their later decades. “Immediately the figure jumps: 120 years, 150, longer. And there’s a strong correlation between someone’s age and how long they say they want to live for: the older you get, the further away you want the deadline. When you survey terminally ill people, in hospices and on their deathbed, the vast majority still have a very strong will to live. In most circumstances, I’d argue, people would like to live longer, but feel it’s not possible.” In essence, as our deadline approaches, few people actually want to die.
It’s a divergence from much received wisdom. Twentieth-century thinkers like Bernard Williams and Viktor Frankl posited that death gives life meaning. It’s an argument Zeleznikow-Johnston offers short shrift. “Some say we need death because it sets a deadline to achieve goals,” he says, “but that’s not compelling.” In his book, he rejects, too, suggested environmental and social benefits of dying, too.
“It’s less that there are strong arguments why death is good,” he argues, “but what I call palliative philosophy: death is inevitable, we want convincing reasons as to why that’s good, so we create them. In fact, we spend vast amounts globally on healthcare and medical research.” It makes up 10% of global economic activity. “Modern medicine is really the practice of trying to keep death at bay. But we haven’t yet acknowledged or agreed – as a society – that the end goal of medical research is actually to eliminate disease completely.”
“In the early 2000s,” he says, “specialists were pushing for urgent debates about AI capability and safety. There was no timeline, but they warned of what was coming.” Their pleas weren’t heeded. “From 2012, AI exploded. Wider society hadn’t talked about it, and now we’re under-equipped and under-prepared.” Zeleznikow-Johnston suspects a similar revolution in mortality is creeping up on us. Even if you dismiss the rest of what he’s advocating, he says, on the topic of “defeating death: good or bad?” we ought to make up our minds. Presuming we opt for the former, Zeleznikow-Johnston reckons he might just have a plan.
Before grappling with the practicalities of extending our lifespans, consider its foundations, he says. “Only when we understand what it is to die, can we consider what it means to keep living. Sure,” he concedes, “if someone developed an anti-ageing drug that halted the ageing process, it wouldn’t need wider discussion.” We’d simply live as we do now, with the prospect of life lasting indefinitely, if we remain out of harm’s way. But this isn’t quite Zeleznikow-Johnston’s vision. His is complex, with any potential payoffs in the distant future. Possibly, he’d see us resurrected in unrecognisable forms. “People assume we have a crisp, clear idea of what death is,” he says, “when that’s not the case: it’s far murkier.”
In his book, The Future Loves You, Zeleznikow-Johnston outlines how the demarcation between life and death blurs. “Until the middle of the 20th century, if you stopped breathing and your heart stopped beating, you were declared dead. No further interventions were available.” Technology changed things. “We developed mechanical ventilators to keep us breathing; machines to keep blood circulating when the heart stops.” Today, life support devices can act as a fully artificial heart and lungs. “These advances pushed us toward a definition of death based on brain activity.”
In 1968, brain death was introduced into clinical practice: the irreversible cessation of brain functions. Once again, scientific advances now suggest this might be defunct. “We see that little bits of brain function, like regulation of body temperature or hormone function, can remain, even when most medics would declare someone dead,” he says. Increasingly, medical innovations will allow for certain brain functions to be replicated artificially. “Prosthetics are returning blood pressure control to spinal injury patients. After stroke or brain damage, implants can let people talk or use limbs. It’s fairly primitive now, but they’ll improve.” Where, then, do we draw the life/death line?
Increasingly, says Zeleznikow-Johnston, experts are turning to identity. “Maybe a real definition of death,” he says, “is when someone’s personal identity – their connectome – is permanently lost.” In layperson’s terms, when our unique consciousness disappears for good. “Most relevant are areas of the brain like the cortex: home to personality and long-term memory.” Much like the total of our genetic makeup is known as our genome, our identity is found in what’s labelled our connectome; the entirety of connections between neurons in our brains. “It can’t be about the physical stuff in our brain,” he says; the cells which make up our body mass continually renew over the course of a lifetime.
Just as it’s the words printed in a book, rather than the specific ink used to form them, that gives its pages meaning, Zeleznikow-Johnston believes the same to be true of you and I. Here lies the heart of Zeleznikow-Johnston’s proposition. “If that’s the case, then what can we do now to preserve these identities, when we can’t currently cure someone’s health issue, but might in the future, if only we could buy some time.”
With current technology, Zeleznikow-Johnston believes, this is already possible; scientifically straightforward, too. There are the obvious examples where we press pause already: sperm, eggs or embryos can be frozen in stasis for decades before being implanted. “What you’re likely less aware of,” he says, “are other analogous surgical procedures already in use. Sometimes, during surgery for aneurysms, or damage to blood vessels around the heart, doctors cannot simply route around with bypasses.” Blood flow in these bodies needs halting if an operation has any chance of success. In normal circumstances, this would prove fatal. For decades, however, surgeons have been circumventing death with a technique known as deep hypothermic circulatory arrest.
“It’s essentially medical hypothermia,” he says. “Cool someone’s body down to around 20C, their heart and brain activity and blood circulation will totally stop.” Essentially, the patient looks dead. Procedures can last 30-40 minutes. “Then once re-warmed, miraculously, most of the time patients are restored to consciousness with cognitive function intact.” After 60 minutes in this state, the risk of brain injury increases. “But it’s a useful precedent: putting people in stasis might be possible if done right, as long as we hold on to those psychological properties inside the connectome.”
Rudimentary efforts to achieve this started in the mid-1960s: American psychology professor James Bedford, the first human to be frozen; cryonically preserved. To date, roughly 600 people globally have undergone a cryonic procedure. “There’s good reason to think techniques used in previous decades are just no good,” argues Zeleznikow-Johnston. “Try to straight freeze a human body or brain, ice crystals destroy the tissue. More complicated versions have been tried, the addition of what’s ostensibly antifreeze, but they’ve led to severe dehydration.” Put bluntly, brains shrivel up. “Obviously, nobody has demonstrated the reversal of the process, and brain tissue preserved this way doesn’t look good under a microscope.”
Now, Zeleznikow-Johnston offers an alternative suggestion: aldehyde-stabilised cryopreservation, also known as fixation. “Essentially,” he says, “by introducing chemicals at the opportune moment which preserve the structure of someone’s brain, we can hold onto its circuitry and structures.”
Once frozen, in essence, preserving our identity indefinitely. “In labs, this process of fixation is used routinely with animal research. Developed in 2015, it’s not a complicated procedure and has been tested on large animals and humans, postmortem.”
Two groups on the US west coast, Zeleznikow-Johnston tells me, are on the cusp of offering this to the public. Another in Europe. “It can certainly be done today,” he’s confident, “and in the next year, it’ll be more accessible. It could be rolled out quickly, if there was demand.”
He tots up rough costs in the book’s closing chapters: at today’s prices, roughly $13,000 should pay for the initial preservation procedure. If done at scale, a further $1,300 annually should account for on-going storage and associated admin costs. “I’m not an accountant,” he adds, “but that’s my best estimate.” Small change compared to the cash required for many medical procedures – from cancer therapies to transplants.
But how we might eventually resurrect remains unclear. What use is pressing pause without a restart button? There, he accepts, we’re firmly into the field of sci-fi. Unfazed, Zeleznikow-Johnston opines that major advances in nanomedicine offer one route; else there’s what’s known as mind-uploading, or mind-emulation – transferring someone to a digital form. “Break down the elements and it’s a fairly straightforward extrapolation from today’s technology,” he says. “Take very high resolution scans of brain structure to characterise how someone’s neurons work, recreate it in a digital format then put it in another robotic, virtual or biological body.” Future scientists will need to fill in the details. “Yet if the memories and experiences which define us are held on to, a person has survived. A robotic or digital brain, if done right, I’d argue, is still you.”
If tomorrow, Zeleznikow-Johnston received a terminal diagnosis, he’d eventually undergo the brain preservation procedure. He’d encourage friends and family to follow. “My fear of death hasn’t been assuaged,” he says. “It still scares me. What I’m proposing isn’t magic, even if it comes to fruition.” Countless variables would need to land in our favour: the tech developed and implemented properly. Nuclear war and climate catastrophe avoided. Some future generation opting to offer their distant ancestors another chance at life. “Even with a guarantee of everyone I love returning, I’d still miss them in the short term, but it does provide some comfort. My existential despair that everyone I love will one day disappear hasn’t gone away completely, but it offers a glimmer of hope.”
Still unconvinced? Just look, he urges, to anaesthesia. “Prior to the mid-19th century, if you needed an operation, you just had to cope with the pain. Yes, you could take some herbs, alcohol; maybe opiates if they were available.” Alternatives included what was, ostensibly, strangulation, else delivering a knockout blow to the patient’s head. “This was the case throughout human history, until the discovery of anaesthesia. It was an unprecedented change. No longer did you have to suffer.”
There’s far from consensus on these topics: much is uncharted territory. A newly published survey of 300 neuroscientists found 40% predict brain preservation and restoration will prove possible. Still, Zeleznikow-Johnston is more than prepared to see his entire thesis shot down. “Sceptics should put in the effort to scrutinise and critically appraise my proposal,” he says, “either proving that what I’m advocating for can’t work – in which case I’ll apologise and abandon it – or they’ll realise what I’m suggesting has merit. It’s time to establish an academic consensus on the current and near-term feasibility of brain preservation.” One thing, however, is for certain: in an instant, what was once believed impossible can become just another fact of life.
The Future Loves You: How and Why we Should Abolish Death by Dr Ariel Zeleznikow-Johnston, published by Allen Lane at £25. Buy it for £22.50 from guardianbookshop.com