My oncologist has one of those little motivational prints hanging on his waiting room wall, with the simple statement, “Trust Your Instincts”. One day, bored with the long purgatory of the waiting room, I tweet this news to the world with the observation: “If I trusted my instincts, I’d run screaming from this place and never come back.”
I’m only half-joking. I don’t wish to appear ungrateful for the miracles of modern medicine, without which I very probably would not be alive. Yet the routine of the oncologist’s visit feels deeply dispiriting.
I sit and wait for anywhere up to an hour or more, in an atmosphere thick with dread and stress and anxiety, whiling away the time on my phone or with a trashy magazine, until my name is called. My oncologist takes a cursory glance at my latest blood test results, usually tells me to continue the medication I’m on, writes me a script for another blood test and tells me to come back in four to six weeks.
The final straw comes about four years after my diagnosis of stage four metastatic prostate cancer, as I stand up to leave another perfunctory ten-minute consultation after an hour’s wait.
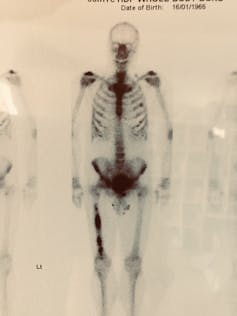
Something just doesn’t sit right about all this. It’s my life hanging in the balance. I have been through radiation therapy (reasonably tolerable), chemotherapy (seriously debilitating), hormone therapy (made me almost suicidally depressed) and surgery (harrowing but quickly over with).

The lack of opportunity for a more wide-ranging conversation about treatment options, how I’m holding up emotionally and strategies to mitigate the life-sapping side effects of treatment just feels wrong.
I walk towards the door, pause, turn and announce, “Oh, one more thing”.
My oncologist does not appear pleased by this development. He has a waiting room full of patients and is already running an hour behind schedule.
“It’s been four years now. I work really hard at this,” I begin tentatively. We’re entering uncharted territory. I’m talking about my feelings and expecting him to respond, a betrayal of our unspoken doctor–patient contract up to this point. I press on regardless.
“I follow a strict diet, exercise and meditate daily, do everything I can to support my health. How do you think I’m going?”
I pose, opening the way for him to offer some soothing words of encouragement. He briefly ponders this unscripted moment, as if I’ve just told a joke he doesn’t quite get.
“About average,” he eventually declares, coolly. “Some of my patients are doing better than you, some worse. You’re about average.”
His response seems designed to ensure I never again have the impertinence to ask such a question, or to attribute any therapeutic powers to my own lifestyle interventions. Even if this was his sincerely held professional view, would it have killed him to say something vaguely positive like, “It’s great that you are being so proactive about supporting your health”? Or a kind-hearted white lie, even if he didn’t actually believe it: “You’re doing great. Keep it up.”
Read more: How kindness can make a difference in cancer care
Emotional distance
I have no reason to doubt my oncologist’s professional expertise and deep knowledge of his chosen field. But I’ve become frustrated by his uninterest in anything I might be doing to support my own health, or any research or suggestions I’ve come across for credible supportive or adjuvant treatments, all of which are swiftly dismissed.
More than anything, I’d like a bit more evidence that he cares, which must be hard to deliver when he’s seeing dozens of patients every day at roughly ten-minute intervals, many with conditions far more dire than mine, most of whom he won’t be able to cure.

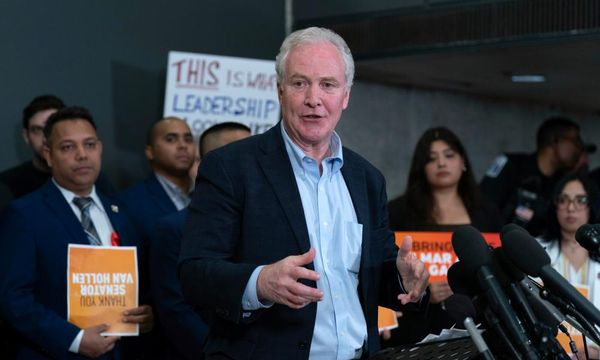
Scottt Morrison reportedly spent almost $200,000 on an empathy consultant for his government, but politicians are not the only ones who need a bit of guidance on reading emotional cues. A 2011 US randomised clinical trial offered oncologists a lecture on good patient communication. Half the group were also offered a tailored CD-ROM presentation to improve their communication styles, recording and critiquing their patient interactions.
The researchers noted the distress and mental health challenges of many cancer patients, observing:
Oncologists frequently miss opportunities to respond to patient emotion and may instead exhibit behaviours that block feelings and create emotional distance.
Report author Dr James A. Tulsky observed:
So often patients aren’t satisfied with the communication they have with their doctor, yet I know physicians care so much about their patients and really want to express that. Physicians may wish to communicate what they are feeling but may not always use the proper words.
The problem here appears to be twofold. Oncologists generally fit a particular psychological profile – disciplined high achievers, able to process and retain vast amounts of highly specialised and technical information and make cool-headed decisions in what are often the most trying circumstances.
People with the skill set to perform these demanding functions might not be naturally inclined towards obvious displays of emotion and empathy. And even if they were, it would be almost impossible to be deeply emotionally invested in every patient. Compassion fatigue is real.
But oncologists also suffer from a terrible physical and mental health profile. Numerous studies have shown they have higher incidence of anxiety, depression and suicide than the general population, and are worse at seeking assistance. It’s difficult to offer emotional support when you’re experiencing psychological distress yourself. According to one US study at the Mayo Clinic up to 35% of oncologists suffer burnout.
Oncologists are faced with life and death decisions on a daily basis, administer incredibly toxic therapies with narrow therapeutic windows, must keep up with the rapid pace of scientific and treatment advances, and continually walk a fine line between providing palliation and administering treatments that lead to excess toxicity. Personal distress precipitated by such work-related stress may manifest in a variety of ways including depression, anxiety, fatigue, and low mental quality of life.
A 2019 study found that over 300 physicians die of suicide in the US every year.
The stigma of depression runs deep in the helping professions and in medicine in particular. Although burnout in oncology is acknowledged, the other stigmatised mental health aspects of medical practice — depression and suicide — are rarely recorded or talked about.“
To compound the problem, oncologists are often reluctant to report mental health issues, considering it a potential blot on their career record. "Physicians have been trained to be perfectionists. They’ve been trained not to ever show any weakness, and they think of mental health issues as weakness,” Anthony L. Back, MD, professor of medical oncology at University of Washington Medical Center, told HemOnc Today, an online journal of oncology and hematology.
Another US study found 30% of oncologists “drink alcohol in a problematic way”, and up to 20% of junior oncologists use hypnotic drugs or sleeping pills.
A 2016 Australian qualitative study on workforce sustainability in oncology paints a similar picture.
Researchers conducted in-depth interviews with 22 medical oncologists at various stages of their careers and concluded:
There is considerable concern here that increased patient volume and intensification – also shown in other studies – will lead to poorer outcomes for both themselves (e.g. burnout), and their patients in terms of the quality of care and support they expect from their medical oncologists.
As one early-career cancer specialist put it:
I think you need to be able to commit that time [to patients] in order to be doing an effective job and if [treatment] becomes a box-ticking exercise … it dehumanises the relationship, which I find a struggle … When there isn’t time to see everyone and you have to rush them out, I think that really wears down that important part of the patient-doctor dynamic.
Read more: You should care about your doctor's health, because it matters to yours
Ironies
In my own case, I eventually took the advice of that wall mounted print in my oncologist’s office and trusted my instincts.
I sacked my oncologist and found a new one more open to discussing my own lifestyle strategies, showing empathy and concern for my mental struggles and quality of life along with my cancer.
Does it strike anyone else as sadly ironic that one of the most dire health issues of our times is presided over by a profoundly unhealthy physician population? The current model of cancer care serves no one’s best interests, leaving complex patient needs unmet and exacting a cruel toll on clinicians. We are all – patients and doctors alike – casualties in the war on cancer.
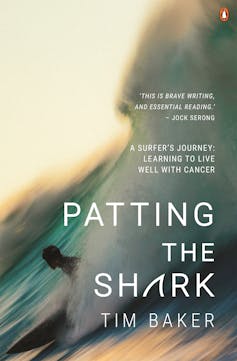
This is an edited extract from Patting The Shark by Tim Baker, published by Penguin Random House Australia, RRP $34.99.
Tim Baker receives funding from Griffith University under a creative writing PhD scholarship
This article was originally published on The Conversation. Read the original article.