For many people living with depression, traditional antidepressants represent either hope or failure — often both.
Antidepressants like fluvoxamine and escitalopram often alleviate depression for a short time before the effects either flatline or crater. Major Depressive Disorder (MDD) that isn’t consistently alleviated by traditional drug therapies is called Treatment-Resistant Depression and as many as 30 percent of people with major depression will develop it.
In recent years, psychedelics like psilocybin, LSD, ketamine, and MDMA have all shown tremendous promise as treatments for people who haven’t responded to traditional antidepressants or other treatments. This is true for depression, people with Post Traumatic Stress Disorder, and even people with terminal cancer. What is less known, however, is exactly how these substances produce such dramatic shifts.
A recent study done by researchers in London and published in Nature Medicine this week may shed light on how these treatments succeed where others fail. fMRI studies of patients with MDD suggest that the antidepressant effects of psilocybin, one of the primary psychoactive compounds in magic mushrooms, may be the result of increased “brain network integration;” identifiable changes in brain activity not seen with traditional antidepressants.
Richard Daws, a neuroscientist and researcher at Kings College tells Inverse, “In healthy adults, psychedelics such as psilocybin and LSD cause the brain to move into an altered state of heightened flexibility and connectivity between systems that are normally more segregated. Now, what's interesting is that in this heightened state of connectivity and flexibility, brain function is almost the exact opposite of what the depressed brain looks like.”
Thus, the researchers hypothesized, that the antidepressant effects of psychedelics might be associated with the changes in brain function produced by the drug.
What the researchers did— Building on research that indicates psilocybin is an effective antidepressant for people who haven’t had a sustained, successful response to traditional antidepressants like SSRIs, researchers at Kings College and Imperial College in London recruited 43 people with severe depression for the study.
Half of the participants received psilocybin; the other half received a conventional antidepressant (participants were not told which they received at the time nor what the traditional antidepressant — escitalopram (or Lexapro)— would be).
The researchers then conducted fMRI brain scans — which capture brain function and active neural pathways in the brain.
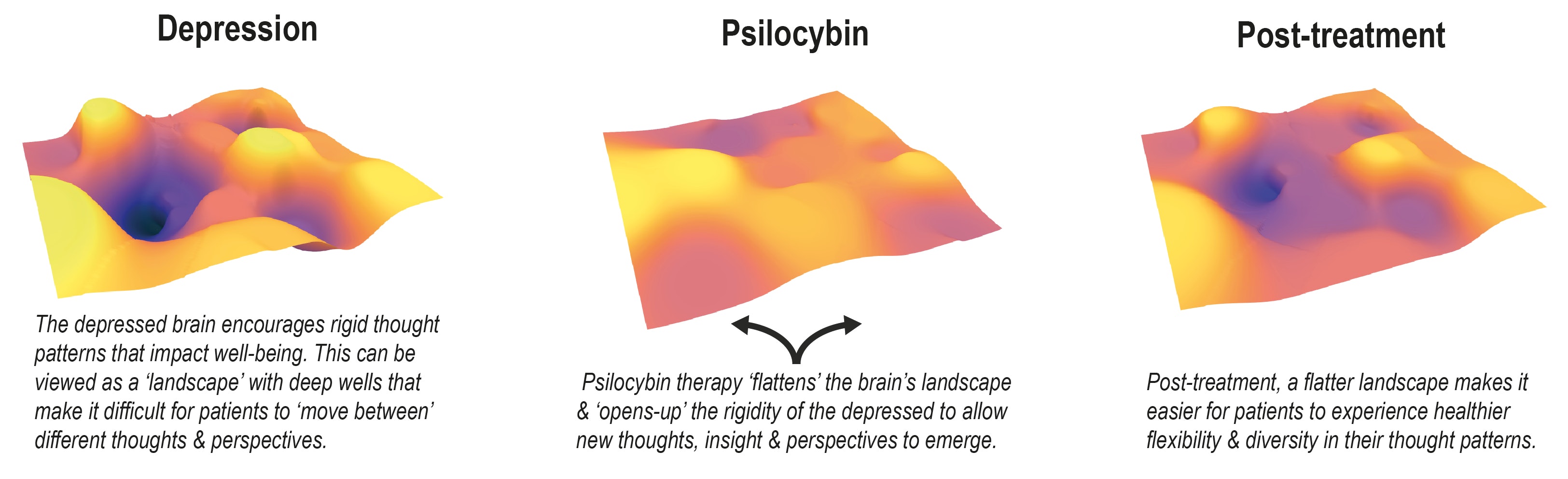
There’s a hypothesis that depression is associated with “cognitive rigidity,” Daws explains, because there’s a “tendency for people with severe depression to get stuck in a rut and to suffer from repetitive negative thinking where they get stuck in a cycle or rigid patterns of thinking.” Three different brain networks are associated with these kinds of thoughts: the default mode network, which is associated with introspective and self-referential thinking; the executive network, which is associated with “cognitive control” and the “salience network” which is associated with identifying relevant stimuli and works with other neural networks to affect communication, social behavior, and self-awareness.
To evaluate the relationship between different systems in the brain, Daws uses an approach called “network modularity,” which “basically tells you how segregated different brain systems are,” Daws says. The fMRI scans before and after the psilocybin treatment could be used with Daws’s method to determine how segregated these networks were in depressed patients prior to the psilocybin treatment and what those same networks looked like following the treatment.
The researchers took one snapshot of the brain activity before receiving the first dose of either the psychedelic or the SSRI and then another three weeks after the final dose.

What they found— The group that had been given the antidepressant escitalopram reported mild improvement in their symptoms, and the scans suggested no major changes in the patients' neural networks before and after treatment.
In the psilocybin group, however, participants not only reported significant alleviation of their depressive symptoms —well beyond what the group receiving the traditional SSRI received — but the researchers also saw dramatic shifts in their second fMRI scan compared to the first. The second scan showed flourishes of activity and heightened connection across many different areas of the brain. In other words, they say significant network desegregation or integration.
The paper included results from a second, smaller experiment that corroborated what the larger study found. In the smaller study, 16 patients with treatment-resistant depression were given psilocybin. As with the larger study, brain scans were taken before and after the psilocybin treatment. The patients’ latter brain scans also showed this heightened connectivity and were correlated with antidepressant effects. Many participants reported they were still feeling the benefit of the treatment six months later.
Furthering the depression and segregated networks hypothesis, Daws explains that the participants who had the most significant changes in terms of network integration also experienced the most significant relief.
Daws says he envisions a depressed brain with a kind of topographical landscape, sharing an image he and his colleagues often use (see below). The worse the depression, the deeper the topographical craters are — or the more segregated the networks — and the harder it is to climb out of them or integrate them with other networks. Psilocybin flattens the topography a bit, making the craters less deep and making it easier for that network to integrate with others.
What’s next— While the findings confirm the fairly well-established antidepressant effects of psilocybin, they also offer exciting insight into the neurological conditions that produce those antidepressant effects. The findings give us insight into the neurological conditions underpinning at least certain kinds of depression. The lack of network integration following the traditional SSRI may also help to explain why so many people don’t respond to traditional antidepressants.
Daws is careful to note this is a small study that needs to be replicated many times over with a larger study group before researchers can draw any definitive conclusions. He’s also quick to explain that the psilocybin was administered in a carefully controlled laboratory setting with multiple psychotherapists guiding the sessions and able to help the participants through any challenging feelings that arose.
“The combined effect of psychotherapist and drug, we think, is an important aspect of helping patients to recapitulate and take new perspectives on important defining features of themselves,” he says. “I wouldn’t advise anyone to do this alone or without medical supervision.”
Going forward, Daws hopes more research will not only confirm the findings but also help clarify the candidates most likely to benefit from psychedelic-assisted therapy.
There is so much need for better treatments for intractable depression and other mental health disorders, Daws says.
“We desperately need large-scale trials,” he says.







