Every Monday, Wednesday, and Friday morning, Carmen Zuniga leaves her house in McAllen before dawn to go to the dialysis center about four miles away. Zuniga has had diabetes for nearly three decades; the disease has left her mostly blind and reliant on dialysis, each session lasting several hours, to stay alive. At the center, she waits in a wheelchair and quietly listens to other patients chatter about family members, meals they’ve eaten, and—more recently—coronavirus and just how seriously to take it. This has been her routine since starting the treatment about three years ago. But her trips to the dialysis center have become far more dangerous as coronavirus spreads rapidly around the country. Now, she worries that the very thing keeping her alive may be what kills her.
Health clinics in the Rio Grande Valley have reduced in-person visits, urging patients to stay home if possible and call in their prescriptions. For many diabetics, who are at higher risk for coronavirus complications, not seeing a medical professional regularly to manage their disease can be risky. For those on dialysis, it’s impossible. Missing even one session can have disastrous consequences. So Zuniga’s only excursions from home these days are to the dialysis center, where she sits in a room with about 20 other people for 12 hours every week. She worries that others aren’t taking the pandemic very seriously, but there’s not much she can do. “Mentally I’m scared, I get anxious,” Zuniga says. “I think I’m gonna die.”
I first met Zuniga, 62, a year and a half ago, when I was writing a magazine story on the crisis of diabetic amputations in the Valley. About one-third of residents have diabetes, triple the national rate, and the region is one of the poorest and least insured in the United States. Many don’t have access to preventive health care, so their diabetes often becomes uncontrolled, leading to complications like blindness, amputations, heart problems, and severe kidney disease that requires dialysis. The lack of access compounds: Uninsured people are more likely to skip medical care, exacerbating underlying health issues. Now, those conditions make COVID-19 more dangerous—but being uninsured means facing even more barriers to treatment if they do get the virus.
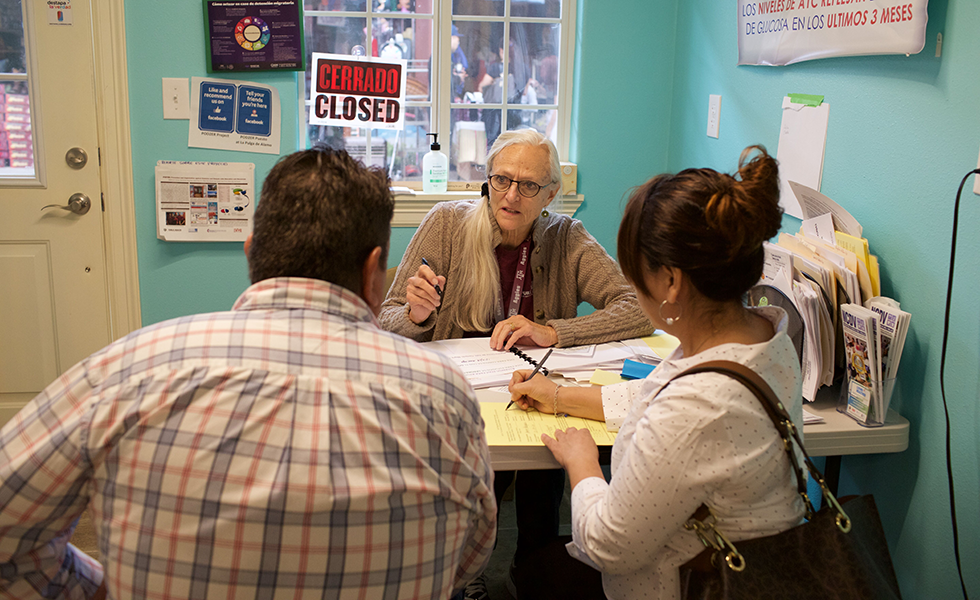
“It’s just a really crazy situation,” says Ann Millard, a retired Texas A&M University professor who has helped run a diabetes screening booth at the pulga, or flea market, in Alamo for years. (The market has been closed for several weeks because of coronavirus.) Theoretically, if testing were more readily available, it would be helpful for uninsured people to know if they have coronavirus even if they can’t afford treatment, so they could isolate themselves from their family, she says. But even that could prove unfeasible: Many, particularly those living in border colonias, don’t have space to isolate, Millard says.
“We’re going to have an incredibly horrendous situation here,” she says. “Tsunami, tidal wave, all those images. And we’re not prepared.”
So far, the four counties that make up the Rio Grande Valley have seen a total of 174 confirmed COVID-19 cases as of Monday morning, according to the state health department. But there are likely many more—testing, which has been extremely slow to ramp up around the country, is particularly limited along the Texas-Mexico border.
Dialysis centers are making changes to try to prevent the spread of COVID-19. At Zuniga’s clinic, nurses take everyone’s temperature when they come in, everyone wears face masks, and no visitors are allowed. DaVita, which runs the clinic and is one of the country’s largest dialysis companies, says it has ramped up infection control and is working on having separate areas or shifts to treat patients with COVID-19.
Zuniga’s whole family is at high risk for coronavirus complications. Her mother and all seven of her siblings have had diabetes—two of them died from the disease. Two of the siblings are nurses at a local hospital. Their mother, nearly 90, had pneumonia last year. She’s living at a nursing home nearby, where her kids haven’t been able to visit because of COVID-19 concerns. David Ceron, Zuniga’s brother, says he’s gone to see his mom through the window, and checks in on Zuniga every so often. “It’s really scary for the whole family,” he says.
The tremendous diabetic population in the Valley means hospitals could be more quickly overwhelmed. “If [coronavirus] does start spreading in that population with kidney disease and diabetes, they will be hospitalized and may spend a lot of time at the hospital,” says Brian Wickwire, chief medical officer at Nuestra Clinica Del Valle, a federally funded community health center. “They will be a major, major contributor to the ICU population.”

Data from the Centers for Disease Control and Prevention released last week shows that people with underlying medical conditions like diabetes have a higher chance of being hospitalized and put in intensive care due to COVID-19.
Zuniga, who was born in the United States, qualifies for Medicare through disability, which covers her dialysis. But many uninsured and often undocumented dialysis patients in the Valley are forced to rely on the emergency room for treatment, which they are generally only able to receive if they’re on the verge of death. If emergency rooms start filling up with COVID-19 patients, Wickwire says, he doesn’t know how hospital staff will handle people who rely on the ER for emergency dialysis.
For medical providers, the solution comes back to preventive health care for everyone, including uninsured and undocumented residents, to avoid these diabetic complications in the first place. “The answer is primary care,” says Wickwire. “So we’re not even having this conversation. … We know that the answer is not more dialysis machines, it’s primary care.”
Find all of our coronavirus coverage here.
Read more from the Observer:
-
Migrants and Advocates Call to Close Detention Centers as COVID-19 Spreads: A new lawsuit argues that an outbreak in detention could overwhelm local health care systems.
-
As Texans are Exposed to Dangerous Pesticides, Lawmakers Aren’t Doing Anything: Pesticide drift is exposing rural Texans to dangerous chemicals. But lawmakers are more concerned with how that is eating into Big Ag’s balance sheet.
-
The Future of Fair Housing in Texas: John Henneberger has spent 45 years advocating for Texans’ right to have a safe, affordable place to live.







