
Maybe you feel worn out. Perhaps you’re also having trouble losing weight. Generally, you just don’t feel 100%.
Could it be Hashimoto’s disease? This common autoimmune thyroid disorder is when your immune system (which fights off viruses and bacteria), mistakenly attacks a part of your body. In this case, it’s your thyroid – a gland located at the base of your neck – and can cause low thyroid hormones levels (hypothyroidism).
Hypothyroidism affects one in 33 Australians and Hashimoto’s is one of the most common thyroid conditions in first-world countries.
While symptoms can be subtle, untreated Hashimoto’s can cause long-term problems with your heart, memory and fertility. Here is what you need to know.
Read more: My scan shows I have thyroid nodules. Should I be worried?
What happens when you have Hashimoto’s?
Your thyroid gland is a butterfly-shaped gland in the neck. It is essential in regulating things like muscle function, digestion, metabolism, the heart and lungs. In children, thyroid hormones are also needed for normal growth and development.
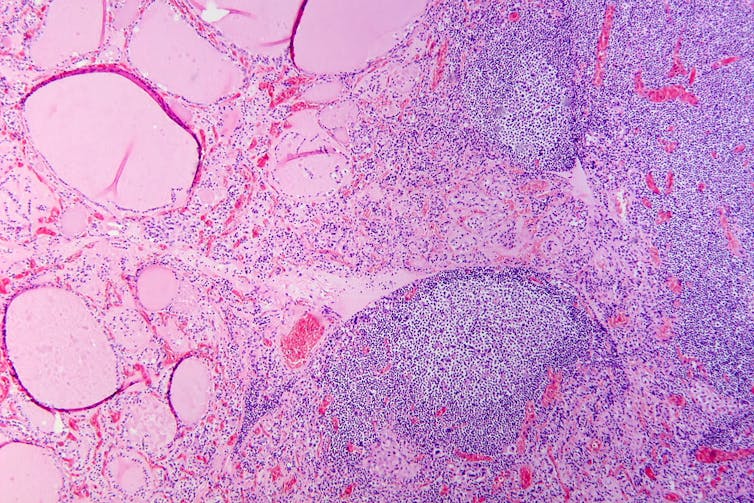
Hashimoto’s thyroid disease, named after the Japanese doctor who discovered it in 1912, is also known as Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis. The disease can cause the immune system to mistakenly produce proteins called antibodies (thyroid peroxidase and thyroglobulin). These can cause inflammation and long-term damage to the thyroid gland. Over time, as thyroid tissue is inflamed and/or destroyed, there can be a decrease in the production of thyroid hormones (hypothyroidism).
Hashimoto’s can present subtly at first. If you only have antibodies with no change in thyroid levels, it is likely you won’t have any symptoms.
However, as the disease progresses, you may experience fatigue, weight gain (or difficulty losing weight), increased sensitivity to the cold, constipation, dry skin, muscle aches, irregular or heavy menstrual cycles, enlarged thyroid (goitre) and occasionally hair loss, including at the ends of your eyebrows.

Read more: Why am I so tired and when is it time to see the doctor about it? A GP explains
What causes Hashimoto’s thyroid disease?
Several risk factors can contribute to the development of Hashimoto’s including:
genetic risk – your risk is higher if you have family members with Hashimoto’s
gender – women are up to ten times more likely than men to develop the disease
age – you are more likely to develop the disease from 30 to 50 years of age
autoimmune condition – having another autoimmune condition like systemic lupus, Type 1 diabetes and celiac disease increases your risk
excessive iodine intake and radiation exposure may also increase risk in people who are already genetically at greater risk.
What are the long-term risks?
Long-term, untreated Hashimoto’s thyroiditis can cause heart issues, higher cholesterol levels, nerve damage (peripheral neuropathy), reduced cognition and infertility.
In pregnancy, Hashimoto’s has a higher risk of pre-eclampsia (high blood pressure affecting several organs), premature birth, placental abruption (when the placenta separates from the inner wall of the uterus before birth) and, in severe cases, pregnancy loss.
The disease has also been linked with an increased risk (but low incidence) of the lymphocytes of the thyroid turning into cancer cells to cause thyroid lymphoma.
How is Hashimoto’s diagnosed?
Diagnosis can be confirmed with a blood test to check thyroid levels and antibodies.
Thyroid peroxidase antibodies are commonly present but about 5% of patients test antibody-negative. In those people, diagnosis depends on the thyroid levels, clinical presentation and ultrasound appearance of general inflammation. An ultrasound may not be required though, especially if the diagnosis is obvious.
Three hormone levels are tested to determine if you have Hashimoto’s.
Thyroid stimulating hormone (TSH) is produced by the brain to speak to the thyroid, telling it to produce two types of thyroid hormones – T3 and T4.
If you have either relative or absolute thyroid hormone deficiency, a test will show the stimulating hormones as high because the brain is trying to get the thyroid to work harder.
Can it be treated?
The management of Hashimoto’s depends on the severity of the thyroid levels. Up to 20% of the population can have antibodies but normal thyroid levels. This is still Hashimoto’s thyroid disease, but it is very mild and does not require treatment. There is no current treatment to reduce antibody levels alone.
Because thyroid peroxidase antibodies increase the risk of abnormal thyroid levels in the future, regular thyroid testing is recommended.
When the thyroid stimulating hormone is high with normal thyroid hormone levels it is termed “subclinical hypothyroidism”. When it is paired with low hormone levels it is called “overt hypothyroidism”. The first is a mild form of the disease and treatment depends on the degree of stimulating hormone elevation.
Overt hypothyroidism warrants treatment. The main form of this is thyroid hormone replacement therapy (levothyroxine) with the dose of the drug adjusted until thyroid levels are within the normal range. This is usually a lifelong treatment but, once the dose is optimised, hormone levels usually remain relatively stable.
In some people with very enlarged thyroid glands causing compressive symptoms (such as difficulty swallowing or breathing), thyroidectomy (surgical removal of the thyroid) is considered.
Hashimoto’s thyroiditis is a common condition caused by your body’s immune system incorrectly damaging to your thyroid and can go undetected. Long-term, untreated, it can cause issues with your heart, cognition, and fertility. It can be diagnosed with a simple blood test. Speak to your doctor if you have any concerns as early diagnosis and treatment can help prevent complications.
Aakansha Zala does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







