A drug-resistant form of fungus is currently spreading through US healthcare facilities and causing alarm, the Centers for Disease Control and Prevention (CDC) has warned.
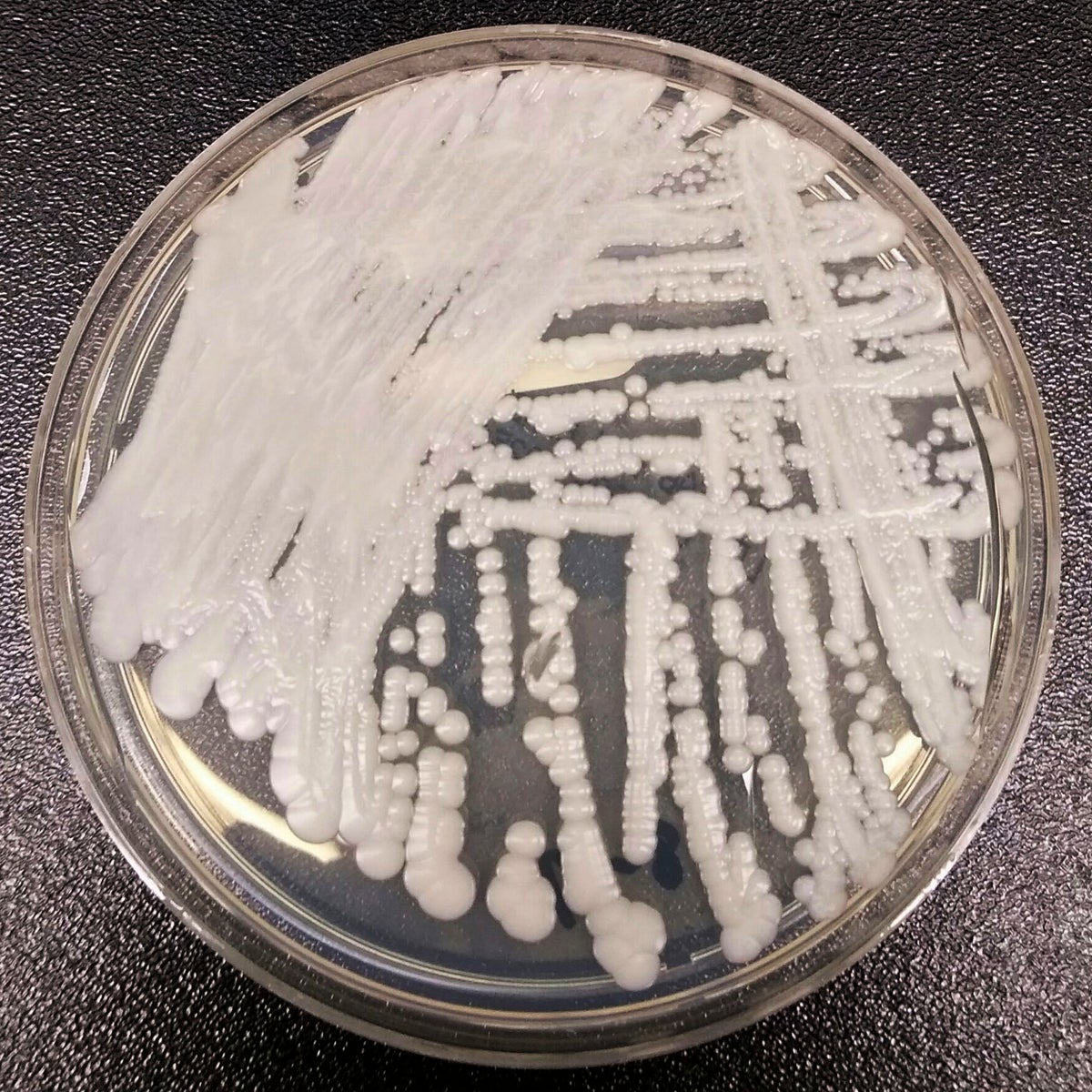
Candida auris or C. auris is a type of yeast that can pose a potentially deadly threat to people with weakened immune systems if it enters the bloodstream and spreads through the body, according to the CDC, with between 30 per cent and 60 per cent of people who get sick in this way dying of their infections.
Patients who have been hospitalised for a long time, have a central venous catheter or other tubes entering their body and those who have previously received antibiotics or antifungal medications are thought to be most at risk, with the infection able to pass from contaminated surfaces and from person to person.
Candida auris requires specialist lab equipment to identify and its resistance to common antifungal drugs makes it difficult to treat, compounding the problem.
The fungus was first identified in Japan in 2009 but has subsequently been traced further back to samples found in South Korea in 1996.
It has since spread to around 30 countries and was first spotted in the US in 2016, causing increased concern after the number of infections rocketed by 95 per cent between 2020 and 2021 from 759 to 1,471 at a time when the world was largely preoccupied with tackling the Covid-19 pandemic.
It has now been found in more than half of American states with Mississippi currently providing particular cause for concern, with 12 cases detected since November and four “potentially associated deaths”, according to State Department of Health spokesperson Tammy Yates.
“Unfortunately, multi-drug resistant organisms such as C. auris have become more prevalent among our highest risk individuals, such as residents in long-term care facilities,” she told NBC News.
The CDC’s new study of Candida auris was led by Dr Meghan Lyman, chief medical officer of the institution’s mycotic diseases branch, who said: “The rapid rise and geographic spread of cases is concerning and emphasises the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control.”
Dr Waleed Javaid, an epidemiologist and director of infection prevention and control at Mount Sinai Downtown in New York, told NBC that the fungus was “worrisome”.
“But we don’t want people who watched The Last of Us to think we’re all going to die,” Dr Javaid said. “This is an infection that occurs in extremely ill individuals who are usually sick with a lot of other issues.”
While the fungus does not currently pose a significant threat to healthy people or communities outside of healthcare settings, its capacity for colonising is a further cause for concern.
“By its nature it has an extreme ability to survive on surfaces,” Dr Javaid said. “It can colonise walls, cables, bedding, chairs. We clean everything with bleach and UV light.”


.png?w=600)




