Parkinson's disease may sometimes start in the digestive tract and make its way to the brain, partly thanks to a chain reaction fueled by gut microbes, new research suggests.
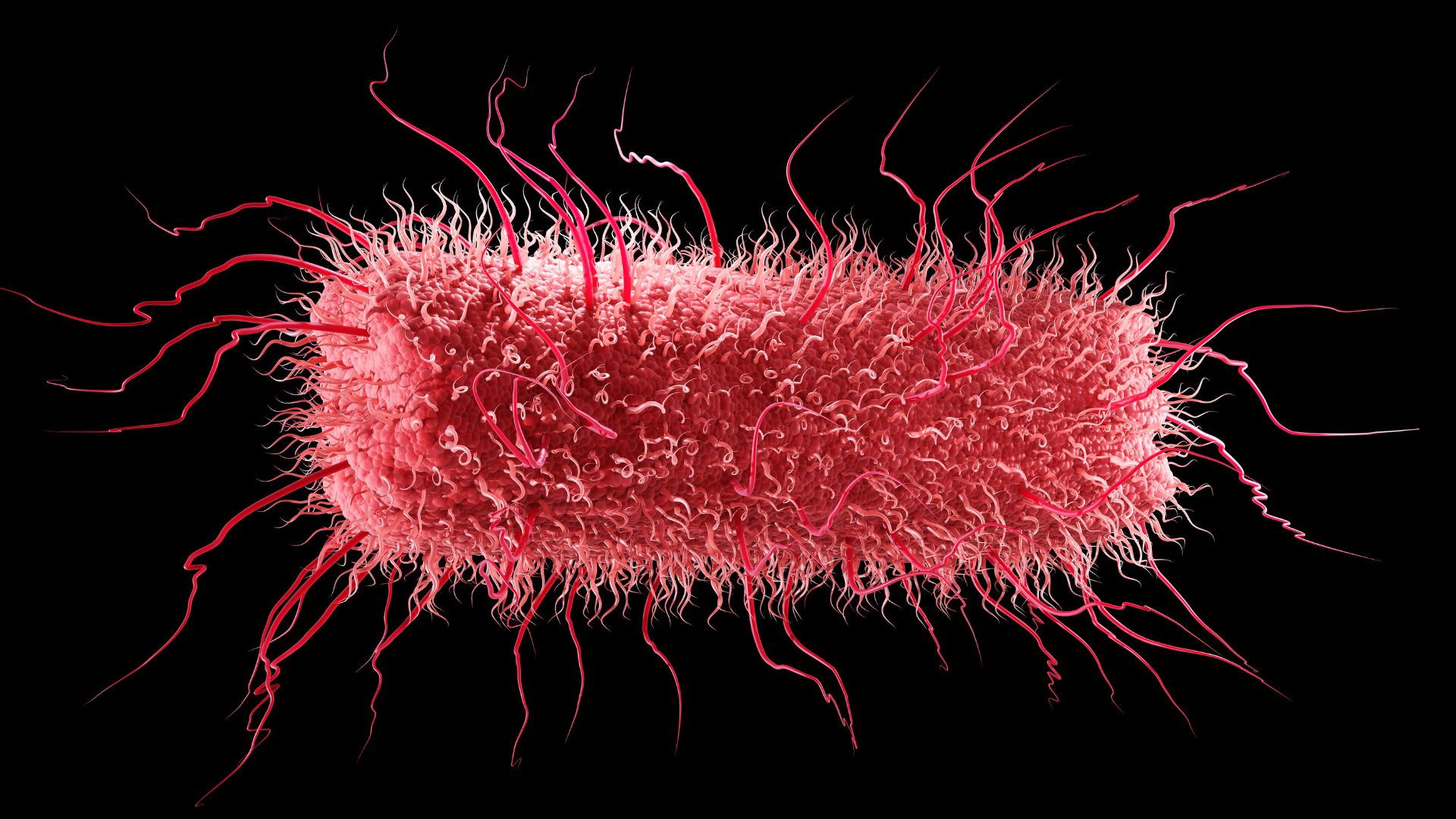
The lower digestive tract hosts many microorganisms, collectively called the gut microbiome. In people with Parkinson's disease, the balance of microbes in the gut shifts, with certain families of bacteria gaining a foothold over others. One family is known as Enterobacteriaceae, which includes the well-known microbe E. coli.
"As there's more Enterobacteriaceae, there's less motor function," said senior study author Elizabeth Bess, an assistant professor in the Department of Chemistry at University of California, Irvine. In short, as the concentration of microbes increases, the movement-related symptoms of Parkinson's worsen, she told Live Science.
Now, in two recent studies, Bess and colleagues have pinpointed a chain reaction that starts with E. coli and ends with abnormal protein clumps forming in the gut — the same protein clumps found in the brains of people with Parkinson's.
Related: Scientists invent tool to see how 'healthy' your gut microbiome is — does it work?
Past research has suggested that, somehow, these clumps in the gut spur the formation of clumps in the brain, perhaps through the nerve superhighway that links the two organs. Thus, the new studies might help unravel how the gut microbiome contributes to that chain of events.
Not all cases of Parkinson's are thought to start in the gut and spread to the brain; some likely do the opposite. "We don't know what fraction is starting in the gut, at this stage," Bess said. But by better understanding the gut-to-brain cases, scientists could potentially uncover ways of preventing this subtype of the disease, she suggested.
The researchers published their findings in March and July in the journals ACS Chemical Biology and ACS Chemical Neuroscience, respectively.
To learn how protein clumps form in the gut, the researchers first looked at past studies of the brain. Cells in the aging brain can accumulate iron that messes with the structure of dopamine, a chemical messenger. That dopamine, in turn, can react with healthy proteins called alpha-synucleins, causing them to clump. The team wanted to see if something similar might happen in the gut, where dopamine is also abundant.
The researchers grew E. coli in a lab dish alongside iron and nitrate, a compound found in the gut when it's inflamed or under oxidative stress. E. coli can use nitrate for fuel, and in the process, it removes one of the nitrate's oxygen atoms, transforming it into another compound, called nitrite.
This nitrite is the key. Once released from the bacteria, the compound reacts with iron, adding oxygen, or "oxidizing" it. The oxidized iron then oxidizes dopamine, and the dopamine reacts with alpha-synuclein, causing it to clump. The researchers watched this clumping unfold in cells from the lining of the mouse gut, which resemble the same type of cells in the human gut.
"Eventually, you get to this aggregation process," Bess said. "Something that's interesting about that to me is that … there's potentially several sites of intervention." Given that there are several steps to get from E. coli to protein clumps, there are several opportunities to stop the process, she said.
In fact, in their ACS Chemical Neuroscience paper, the team found that a compound in coffee — caffeic acid — can help stop the iron from oxidizing dopamine. The researchers think the concentrations of caffeic acid they worked with mimic what might be found in a coffee drinker's gut, but that hypothesis will need more testing to confirm, Bess noted.
Taken together, the studies are an early step toward explaining how the gut microbiome might contribute to Parkinson's.
Vinata Vedam-Mai, an assistant professor of neurosurgery at the University of Florida who was not involved in the work, called the findings "intriguing." However, she noted in an email to Live Science that the data were all gathered in lab-dish experiments, "without the presence of other cells and immune components."
The findings do suggest that oxidation reactions in the gut might help set off the protein-clumping process the researchers described, Vedam-Mai said. But there are many other things mingling in the digestive tract, including antioxidants from people's diets and waste products released by immune cells. Because of this complexity, "I doubt that nitrate metabolism is one of the main drives" underlying the oxidation reactions in the gut, she said.
Bess added that, since they were focused on just E. coli, they didn't capture how the bacteria might be interacting with other gut microbes — of which there are many.
Ultimately, "it would be important to test these hypotheses in preclinical models before we take steps toward preventative approaches, or make any substantial statements," Vedam-Mai said. Preclinical models may include lab animals or miniature, lab-grown versions of human organs, for example.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!







