The COVID-19 pandemic transformed over the past five years from a catastrophic threat that has killed over 7 million people to what most people regard today as a tolerable annoyance that doesn’t require precaution. Nonetheless, COVID-19 continues to kill over 2,000 people per month globally and cause severe illness in the infirm or elderly.
The evolution of the COVID-19 pandemic – from devastation, to optimism for eradication, to persistent, uneven spread of disease – may seem unprecedented. As an infectious disease doctor and medical historian, however, I see similarities to other epidemics, including syphilis, AIDS and tuberculosis.
Vaccines, medications and other biomedical breakthroughs are necessary to eliminate epidemic diseases. But as I explore in my book, “Persisting Pandemics,” social, economic and political factors are equally important. On its own, medical science is not enough.
Syphilis, AIDS and TB have stuck around
Syphilis is a sexually transmitted disease first identified in 1495. It causes skin rashes and may progress to causing paralysis, blindness or both. For centuries, syphilis weakened nations by disabling parents, workers and soldiers in the prime of their lives. Innovative drugs – first Salvarsan (1909), then penicillin (1943) – offered a path toward eradication when used together with widespread testing.
Public health programs conducted from the 1930s through the 2000s, however, failed – not because of the efficacy of the treatments but because of socioeconomic conditions.
One challenge has been persistent stigma around getting tested for the disease and tracing sexual partners. Poverty is another; it can force women into commercial sex activities and prevent people from learning how to protect themselves from sexually transmitted infections. Population migration due to commerce or war can cause high-risk behaviors such as sexual promiscuity. Women in some cultures lack authority to negotiate for condom use. And governments have not consistently prioritized the sustained funding needed to support efforts to eliminate the disease.
Despite societal indifference toward syphilis, in the 2020s over 8 million new cases occur globally each year, particularly among racial minorities and low-income populations.
The history of HIV/AIDS is shorter than that of syphilis, but the trajectory has similarities. Doctors first described HIV/AIDS in 1981, when it was a nearly uniformly fatal sexually transmitted disease. Novel antiretroviral drugs introduced in 1996 offered medical scientists the hope of disease elimination through public health campaigns, centered on widespread testing and treatment, implemented in 2013.
But these programs, for reasons like with syphilis, are not meeting their treatment targets across all countries, especially among low-income populations and racial minorities. Sustaining funding for health care infrastructure and the multidrug regimens for 39 million people living with HIV poses an added challenge. Today, despite a cavalier public attitude toward the disease, AIDS causes over 630,000 deaths globally. That number will likely increase substantially given the Trump administration’s decision to cut funding for United States Agency for International Development programs.
Tuberculosis is a third disease that also depleted workforces and weakened nations, particularly in postindustrial revolution 19th-century cities. The disease spread widely because poverty placed people in poorly ventilated working conditions and crowded tenement dwellings. The development of new combination antimicrobial drug regimens offered an avenue for disease eradication in the 1960s.
Nonetheless, the inability to sustain funding to complete complex treatment courses, problems isolating people who could not afford suitable homes, and poor adherence due to homelessness, incarceration or migration during war or trade have compromised public health campaigns. Despite societal nonchalance, tuberculosis today kills up to 1.6 million globally yearly.

The COVID-19 case study
The trajectories of these epidemics show how campaigns based solely on biomedical approaches that target pathogens are not enough to eliminate disease.
COVID-19 provides the latest example. In the U.S., the pandemic and its lockdowns disproportionately affected low-income people and racial minorities, especially those employed in front-line jobs that did not allow remote work from home. These groups were more likely to reside in crowded residences with poor ventilation or no space for isolation.
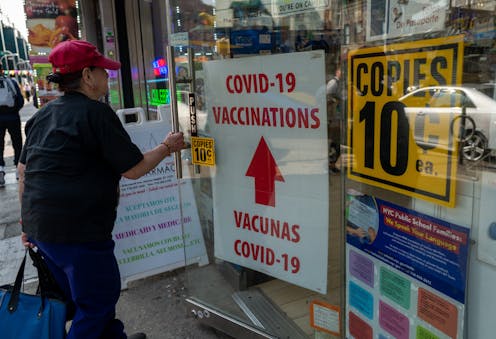
Despite the rapid development of a breakthrough mRNA vaccine that offered hope for what President Joe Biden euphorically termed “independence from the virus,” the promise never fully materialized.
Too few people received shots, in large part due to socioeconomic factors.
Wealthy countries purchased vaccines that lower-income countries could not afford. Allocation difficulties kept vaccines from remote regions of the world.
Vaccine hesitancy due to mistrust in science, along with sentiment that vaccine mandates violated individual freedoms, also prevented people from getting the shot. Similar attitudes reduced rates of mask-wearing and isolation.
Consequently, surges that could have been avoided took more lives.
Drugs and vaccines can’t do it alone
Modern medical science is unmatched in treating pathogens and disease symptoms. But to stop disease, it’s also critical to address the social, economic and political conditions that enable its spread.
Public health officials have started to implement a variety of structural solutions:
- Stigma reduction programs to reduce the shame of having a disease and increase the number of people tested.
- Cash transfers to provide sex workers with capital to invest in less risky, alternative businesses.
- Peer education to empower sex workers with the authority to negotiate for condoms and safer sex practices.
- Health infrastructure expansion to enable access to testing and treatment facilities.
- Housing reforms to guarantee adequate air filtration and appropriate isolation facilities.
- Resistance to anti-science appointees to government positions to prevent the implementation of regressive public health measures.
- Sustained funding for public health efforts across political administrations that may have different priorities.

Early 20th-century public health officials had hoped that efficient scientific solutions alone could take the place of 19th-century, pre-germ-theory environmental sanitation efforts. COVID-19, syphilis, HIV/AIDS and tuberculosis show that while biomedical breakthroughs are necessary to eliminate epidemic diseases, sustained focus and resources aimed at helping the most socially and economically vulnerable are essential.
Powel H. Kazanjian does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







