More than 53,000 Americans are projected to die from colorectal cancer this year. Although colorectal cancer is the second-most common cause of cancer deaths in the United States, it can be cured if caught early. Detecting a tumor as soon as possible can help you get treatment as soon as possible, giving you the best chance for survival.
In my work as a gastroenterologist, I treat patients from every background and walk of life. Uniting them are a growing number of insurance barriers threatening access to timely care. All too often, payers take a long time to make coverage determinations, or they even deny them outright.
With the alarming rise of colorectal cancer diagnoses among Americans under 50, it is more important than ever for people to know their cancer risk and when to get screened.
Here are common questions I and other gastroenterologists get from patients about colorectal cancer:
What is my colorectal cancer risk?
Anybody at any age can develop colorectal cancer. However, some people may be more likely to get the disease than others.
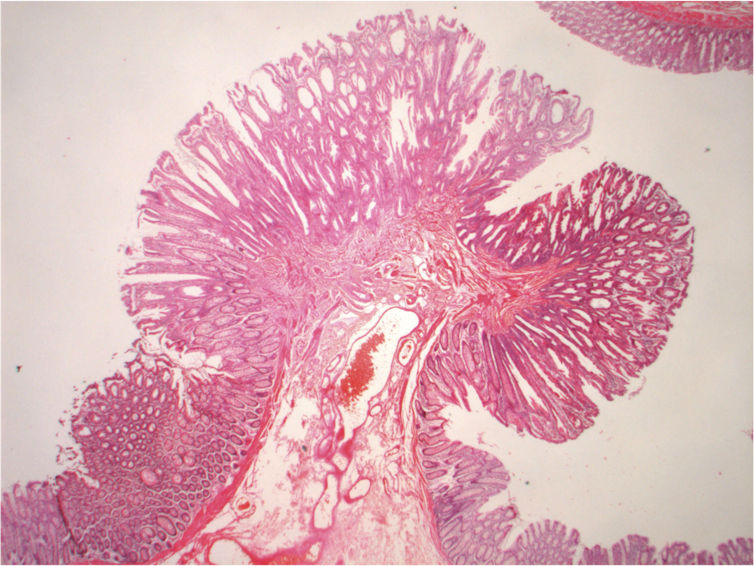
For example, people with a family history of colorectal cancer or a personal history of polyps, which are abnormal growths in the tissue of the colon or rectum, may have a higher risk.
Inflammatory bowel diseases like Crohn’s and ulcerative colitis can also increase your risk of developing colorectal cancer. This is because the chronic inflammation associated with these diseases can promote the development of abnormal growths.
Race and ethnicity may also affect colon cancer risk. Black and Indigenous Americans are significantly more likely to develop – and die from – colorectal cancer. While genetics does play a role in disease development, much of the risk of colorectal cancer is linked to environmental factors. These include a person’s income level, types of food and groceries available in the neighborhood, access to primary care providers and specialists, and a wide variety of other social determinants of health.
Lifestyle factors like smoking, not exercising regularly and poor diet can also increase your colon cancer risk. Researchers have shown that red meat releases chemicals that can cause inflammation, while high-fiber foods and vegetables can help lower inflammation. Similarly, a sedentary lifestyle can also increase inflammation. Smoking can lead to harmful genetic changes in colon cells.
What are my screening options?
People with colorectal cancer usually don’t exhibit symptoms until the disease progresses to a later stage. That is why early and regular screening is critical.
The U.S. Preventive Services Task Force recommends Americans begin regular screenings at age 45. Recognizing that the incidence of colorectal cancer has grown among younger adults, the task force lowered the age from 50 in 2021. Screening may start earlier and occur more frequently for people who have an increased risk of colon cancer.
There are various screening methods, and your medical provider can recommend procedures based on your risk factors.
Many people choose to get a colonoscopy, which is a screening test that can also prevent cancer by removing precancerous polyps. It involves using a long, flexible tube with a light and a camera on the end to visually inspect the colon for signs of cancer, abnormalities in the colon lining, or growths such as polyps. Ultimately, colonoscopy screening can significantly reduce the incidence and mortality of colorectal cancer.
Other screening strategies include noninvasive stool testing, imaging scans and a combination of endoscopic visualization with stool-based testing.
Your doctor can help you select a test that aligns with your preferences, values and risk factors. Suggested screening approaches in people with an average colon cancer risk include a colonoscopy every 10 years, stool-based testing every one to three years, or CT scans every five years for those who are unable to have a colonoscopy as an initial screening test. A positive test result for these alternative approaches should be followed by a colonoscopy.
With routine screening, one out of every three colorectal cancer deaths can be avoided.
Why won’t my health insurance pay for my colonoscopy?
While colorectal cancer screening is free as a preventive service under the Affordable Care Act, some insurers are making it harder for people to get care.
For example, Blue Cross Blue Shield of Massachusetts proposed a 2024 policy that would have deemed the use of anesthesia in endoscopies, colonoscopies and other vital procedure as medically unnecessary. This meant patients would have had to pay out of pocket to cover the anesthesia needed for colorectal cancer screenings, potentially creating major cost barriers. The insurance company only reversed course after an outcry from physicians and patients.
Another troubling trend is expanded use of prior authorization, a process some health insurers use to determine if they will cover the cost of a medical procedure, service or medication. Insurers can delay or deny coverage of medically necessary care that physicians and medical guidelines recommend because they deem certain health care services unnecessary for a patient or too expensive to cover.

In 2023, UnitedHealthcare proposed a policy that would have required the 27 million people under their plan to obtain insurance approval before they could get diagnostic or follow-up colonoscopies. After protests from physicians and patients, the insurer put the policy on hold.
UnitedHealthcare has also made plans to introduce a program in 2024 that could involve prior authorization for colonoscopies. The insurer has released little information about why it feels such requirements are necessary, what services would require prior authorization and how it would protect patients from unnecessary delays and denials.
How can I lower my risk of colorectal cancer?
If you haven’t already, look into getting screened for colorectal cancer. Talk with your doctor’s office and check with your insurance company to understand what will be covered before your procedure. If you’re 45 or older, a colonoscopy can screen for and prevent colorectal cancer.
Younger adults can take steps to reduce their risk of colon cancer by adopting healthy eating and lifestyle behaviors. Being aware of personal risk factors and seeking medical attention for symptoms – such as changes in bowel habits, rectal bleeding, abdominal pain or unexplained weight loss – can help you discuss screening options with your health care provider.
If you have already had a colonoscopy and had polyps removed, make sure you know when you are due to return for a follow-up colonoscopy. It could save your life.
Andrea Shin is affiliated with the Rome Foundation and the American Gastroenterological Association.
This article was originally published on The Conversation. Read the original article.