The first UK baby with DNA from three people – mother, father and a female donor – has been born after a groundbreaking IVF procedure known as mitochondrial donation treatment (MDT).
This procedure aims to prevent children from inheriting harmful mutations their mothers carry and are likely to pass on to their children. Babies inherit all their mitochondria from their mother, so harmful mutations in the “batteries” can affect all of the children a woman has, reported The Guardian.
In such cases with unhealthy mitochondria, natural conception is often a gamble. Some babies might be born healthy while others may inherit and develop severe, progressive and fatal diseases.
The baby born from this procedure has DNA from the mother and father as usual, plus a small amount of genetic material (about 37 genes) from the donor. More than 99.8% of the DNA in the babies comes from the mother and father.
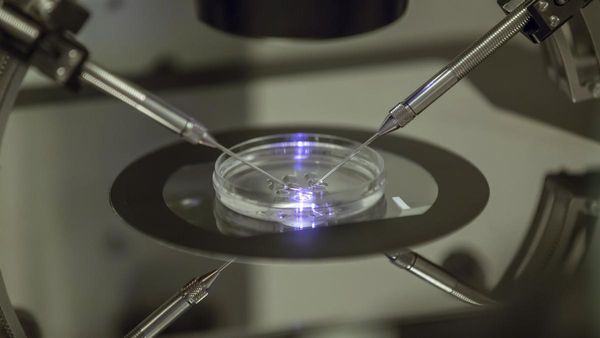
Research on MDT, also known as mitochondrial replacement therapy (MRT), was pioneered in the UK by doctors at the Newcastle Fertility Centre. In this procedure, first, sperm from the father is used to fertilize eggs from the affected mother and a healthy female donor. The nuclear genetic material from the donor’s egg is then removed and replaced with that from the couple’s fertilized egg, reported The Guardian.
The resulting egg has a full set of chromosomes from both parents, and carries the donor’s healthy mitochondria instead of the faulty ones from the mother. This is then implanted in the womb.
This procedure is also not without risks. Recent research has found that in some cases, the tiny number of abnormal mitochondria that are inevitably carried over from the mother’s egg to the donor egg can multiply when the baby is in the womb. This could lead to a disease in the child.
“It’s exciting news, but at the same time it doesn’t tell us anything about whether the method has actually worked,” says Dagan Wells, a reproductive geneticist at the University of Oxford, UK told the journal Nature. “There are open questions, and we need to get answers as soon as possible,” Wells added.