Back in the 1990s, two major drug developers — SmithKline Beecham (now GlaxoSmithKline) and the publicly owned Canadian drug manufacturer Connaught Labs — were sprinting to create a vaccine for an infectious disease that seemed to pop up out of nowhere in the northeastern United States in the mid-to-late 1970s.
In 1975, a cluster of children and adults in Lyme, Connecticut, complained of arthritis-like symptoms that doctors couldn’t pin down. By 1982, as more cases had mounted, researchers identified a bacterium, Borrelia burgdorferi, as the infectious culprit, which they also found was transmitted through tick bites, particularly the poppy seed-sized black-legged “deer” tick. By the late 1990s, Lyme disease amounted to over 15,000 confirmed cases a year. A vaccine was sorely needed.
While both vaccines in development targeted a protein called outer surface protein A carried by the Borrelia burgdorferi bacterium, SmithKline’s LYMErix won out in clinical trials. The FDA swiftly approved LYMErix in 1998, but its success was short-lived. A 2000 study suggested the jab caused autoimmune arthritis in hamsters, and some LYMErix recipients publicly complained of joint pain (though the FDA never found a connection). Then, after a class-action lawsuit, SmithKline Beecham pulled the vaccine from the market in 2002.
Over the past twenty years, Lyme disease cases have continued to climb, and we are finally tantalizingly close to another vaccine.
Lyme disease cases could skyrocket in the coming decades
The infectious disease is expanding its borders beyond the northeast and midwest US and northern regions of Europe and Asia, where it’s typically considered endemic. In the US, the incidence of Lyme disease has nearly doubled since 1991, from 3.74 reported cases per 100,000 people to 7.21 reported cases per 100,000 people in 2018, according to the CDC. This is due to the rising temperatures accompanying climate change, making our planet more hospitable for the black-legged tick and its Lyme disease-carrying kin.
Over the past twenty years, Lyme disease cases have continued to climb, and we are finally tantalizingly close to another vaccine.
In a repeat of history, two major biopharmaceutical companies — Pfizer and Moderna — are in a race to develop a Lyme disease vaccine for our modern times. Still, many infectious disease experts Inverse spoke to say it won’t be enough. Better diagnostic testing and treatments will be crucial, too.
The new vaccines: A little bit of old and a lot of new
The current approach to a Lyme disease jab is still to target the outer surface protein A.
This protein helps bacteria of the Borrelia family stick to the tick’s gut when it passes from an animal reservoir — small mammals like the white-footed mouse and ground-dwelling birds are common ones — to the insect during feeding. Once the tick latches on to an unsuspecting human (or animal like a dog) for its next blood meal, the bacteria turn off the protein (since it no longer needs to stick to the tick) and schmoozes over to its new host.
In a repeat of history, two major biopharmaceutical companies — Pfizer and Moderna — are in a race to develop a Lyme disease vaccine for our modern times.
There’s quite a bit of a lag between when the tick latches on and when the bacteria gets passed through a bite — about 36 to 48 hours. If someone is immunized against the bacteria’s outer surface protein (and has antibodies at the ready), this gives enough time for the antibodies in the host’s blood to get into the tick’s gut and prevent transmission before starting the whole Domino effect of infection.
In April, Moderna unveiled two mRNA-based vaccines it's working on: mRNA-1982, which targets Borrelia burgdorferi, responsible for the majority of Lyme disease cases in the US, and mRNA-1975, offering protection against four Borrelia species causing Lyme disease in Europe as well as the US.
“There’s more variability in this particular protein in the European [Borrelia] strains,” Linden Hu, professor of Immunology at Tufts Medical School, who is working with Moderna on its vaccine development, tells Inverse. “In order to have a vaccine that works in Europe, they have to include more [and] different antigens into any vaccine you’re going to use, whether it’s a protein-based vaccine the way Pfizer is doing right now or an mRNA vaccine as we’re attempting.”
Pfizer has been working with French biotech company Valneva to create VLA-15, a jab containing six variations of the outer surface protein A’s most common in strains in the US and Europe. The protein isn’t an exact match since the segment thought to cause autoimmune responses has been engineered out (Hu says this was done out of an abundance of caution given the complaints against LYMErix, despite studies finding no direct link between the jab and autoimmune side effects). Pfizer/Valneva’s vaccine is currently undergoing late-stage clinical trials (a Phase III clinical trial started last August), and the manufacturers are planning to submit an application to the FDA in the next two years for its Lyme vaccine.
Interestingly, if you are a dog, you already have access to a great Lyme disease vaccine that’s been around for a while. This one jab targets the outer surface protein C instead of A. It’s a protein that’s also found in human infections, but Hu says it’s more difficult to create a human vaccine targeting this protein: Unlike protein A, protein C is a bit more multiversal with a lot more variability lending to slightly different variants. You would need to target a majority of protein C’s variants to develop an efficacious vaccine, which is easier said than done. That hasn’t stopped scientists from trying, though. A few studies have been trying to work out the kinks, and one experimental vaccine appears to be effective, at least in mice.
While these jabs focus on sequestering the bacteria before it can cause infection, other scientists are tackling Lyme disease prevention from a different angle by immunizing us against tick bites altogether, Nadine Bowden, a Lyme disease program officer at the National Institute of Allergies and Infectious Diseases (NIAID), tells Inverse.
This approach, spearheaded by researchers at the Yale School of Medicine, involves targeting the tick’s own salivary proteins released through an open wound. The mRNA vaccines are designed so that the immune system recognizes these proteins as foreign invaders and sets off a strong immune response at the site of the bite.
The vaccine is still in the early stages of development and is being tested on guinea pigs. Once it does become available, it could be used not just on us but the animal reservoirs the ticks feed on, like deer or wild mice, preventing the ticks from getting infected and passing it to other non-infected animals.
Prevention through prophylaxis
While a vaccine would provide long-term protection, experts say it alone won’t be enough. Not everyone is going to want to get a vaccine, Mark Klempner, a professor of medicine and former executive vice chancellor for MassBiologics of UMass Chan Medical School, says. He acknowledges that we need to have other options.
For the past several years, he and his colleagues have been working on a therapy that would provide instant immunity before, say, going on a nature hike or vacation to a place roaming with ticks. He calls it pre-exposure prophylaxis for Lyme disease (or Lyme PrEP).
“We knew back [after the LYMErix] vaccine that an antibody was necessary and sufficient for protection,” Klempner tells Inverse. “Once we had [the right antibody], we had a medicine that people could use for immediate protection, unlike a vaccine.”
How long it takes for your body to make antibodies varies depending on the vaccine type. Inactivated or subunit vaccines may require multiple doses over several weeks to stimulate a strong immune response. mRNA vaccines work faster, generating a rapid response, with antibodies appearing within days to weeks, peaking a few weeks after vaccination.
Klempner says that with human monoclonal antibodies against Lyme disease — a single antibody against outer surface protein A is effective against three major Borrelia species in the US — an individual could become naturally immune within days with just one shot versus much longer with multiple shots expected with the Lyme disease jabs in development.
The immunity isn’t long-lasting, but Klempner says Lyme PrEP would address the needs of individuals who need quick immunity for only a short period of time (like vacation goers) and individuals who are immunocompromised. It could also be used in combination with Lyme disease vaccines once someone gets their full round of vaccines of the season.
“I think you could mix and match over seasons,” says Klempner. “You wouldn’t take it the same year [as when you got vaccinated]... you can take our Lyme PrEP antibody, and that will protect you for the next season.”
Clinical trials for Lyme PrEP are still ongoing, but Klempner is hopeful the preventative shot will be available by the latest 2025.
A dire need for better testing
Vaccines and PReP address one side of the Lyme disease coin, which is prevention. But prevention, as well as saying anything about a vaccine’s efficacy, is only as good as our means of determining it. A problem currently facing Lyme disease diagnostic testing is that it’s not as fast or as sensitive as we need it to be, thereby undermining our ability to accurately monitor, track, and treat the infection.
“We’re using the same diagnostic tests that we’ve been using since 30 years ago, and it’s really not very good,” Monica Embers, director of Vector-Borne Disease Research at the Tulane National Primate Research Center, tells Inverse. “The test that we use is called a two-tier test [looking for antibodies against Borrelia] — it’s highly specific, so there aren’t many false positives, but it’s very poorly sensitive.”
Depending on the time between the tick bite and when someone gets their blood tested, the test’s sensitivity could range anywhere between 40 and 60 percent, which isn’t great.
On top of that, it’s not directly testing for bacteria but whether you have antibodies, which doesn’t necessarily equate to an active infection. It also doesn’t really tell you how long ago the person was infected, especially as many tick bites can go unnoticed and are not necessarily accompanied by the characteristic rash (known as a bull’s eye rash), high fever, joint pain, or flu-like symptoms, not to mention full-blown Lyme disease if not timely treated with antibiotics like amoxicillin or doxycycline.
“The problem is that [the bacteria], once they get into the blood from the tick, they disseminate very rapidly and enter the tissue,” explains Embers. “They’re out of the bloodstream pretty quick, so it’s hard to have a direct diagnosis when you can’t find it in the blood.”
While there’s research looking into characterizing different immune chemicals released by the body during a tick bite, Hu and his colleagues at Tufts Medical School are devising a diagnostic test that uses the bacteria’s dietary habits against itself.
Like all cells, bacteria have a cell membrane that’s made up of different molecular bricks, like proteins and lipids. Often, bacteria manufacture their own bricks using the blueprint instructions embedded in their genome. Members of the Borrelia family, however, steal molecular bricks called phospholipids from their host, Hu, and his colleagues found.
“We realized that if you’re putting a host phospholipid on a bacteria, will that now generate an antibody response because now it’s being recognized as foreign?” says Hu. “So that started us looking for antiphospholipid antibodies, and we did find these antibodies.”
Hu and his colleagues found that as long as the bacteria lingered in the body, so too did these antiphospholipid antibodies, vanishing the moment the bacteria does. This quick disappearance could be especially helpful in saying whether someone’s cleared the infection for sure and who may be more likely to have persistent Lyme disease, even after treatment, what’s called post-treated Lyme disease syndrome.
“I think this test would be an adjunctive test. I think you would still need to do traditional testing that would show you that you’ve encountered Lyme disease in the past,” says Hu. “This could help tell whether it's acute or not, whether you still have it or not. It would be a nice complement to existing testing.”
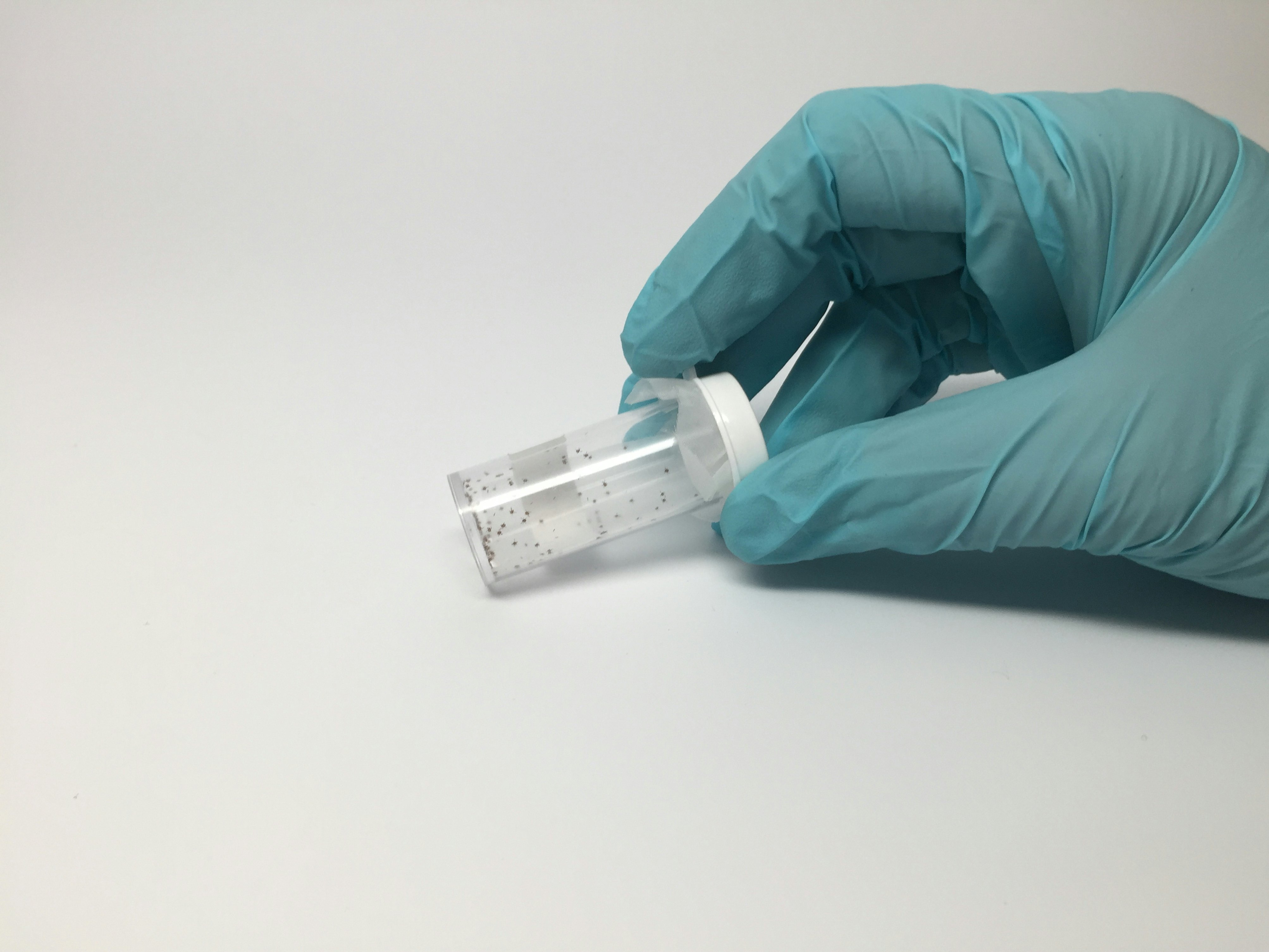
Other researchers are working on at-home test kits that would detect bits of the Borrelia bacteria in pee or slapping a sticker on a tick bite that would change color if got infected, Newsweek reported last month.
The future of Lyme disease
There’s a lot of hope riding on the horizon for preventing Lyme disease. While most of the focus is on prevention, there’s also research into why certain individuals develop post-treatment Lyme disease syndrome, also known as chronic Lyme disease, a condition that affects a minority of individuals who have been treated for Lyme disease. It refers to a set of persistent symptoms like fatigue, joint and muscle pain, and cognitive issues that continue after the initial antibiotic treatment for Lyme disease, despite the absence of active infection.
“I would say we’re still in the dark, there’s not a lot of clarity about what’s causing [post-treatment Lyme disease syndrome],” says Hu. “There’s not a lot of evidence that the bacteria survive after antibiotics, although it’s possible. It’s possible that parts of bacteria still stay in the body even after the bacteria have died, and those are maybe activating the immune response.”
Embers is hopeful that with better diagnostic testing, preventatives, and more effective therapies for individuals living with post-treatment Lyme disease syndrome, we can alleviate the burden of the disease, but only if we rouse up enough interest.
“I chaired the diagnostics sub-committee [of the U.S. Department of Health and Human Services’s Tick-Borne Working Group], and we didn’t find that wasn’t enough research on better diagnostics,” she says. “What we found was that there’s a lot of small labs doing research. They have good ideas and results, but there’s nothing to propel them to commercialize a product. There’s no investment — we really need to get the interest and investment of Big Pharma in better diagnostics.”
As the planet warms and ticks roam free, here’s hoping we solve this epidemic just in time.