On 8th May 1994, Thalassemia International Federation (TIF) observed World Thalassemia Day in memory of George Englezos. George was the son of the TIF founder, who lost his life due to thalassemia. Thalassemia as a disorder and its advocacy around all sectors, such as preventative awareness, healthcare, education, livelihood, and early interventions, have evolved dramatically. In India, thalassemia, along with two other blood disorders, was recognised as a benchmark disability in the Rights of Persons with Disabilities Act, of 2016. This brought a landmark shift in recognition and advocacy for thalassemia that went beyond the health sector and preventative awareness. In the present context, thalassemia and other blood disorders are becoming part of the invisible disability discourse.
Understanding Thalassemia
A large section of the population doesn’t understand thalassemia. In simple terms, thalassemia is a genetic-blood disorder that requires people to have regular blood transfusions mostly throughout the span of their life. However, it gets increasingly complex as we get into the specifics of the disorder. Thalassemia is part of a group of disorders called hemoglobinopathies. Hemoglobinopathies are a group of disorders that are passed down through families (inherited) in which there is abnormal production or structure of haemoglobin molecules. Thalassemia, Hemophilia and Sickle Cell Disorder all come under the umbrella of hemoglobinopathies.
In thalassemia, the presence of haemoglobin is severely low which results in the damaging of Red Blood Cells immaturely. This results in a low count of RBCs and the constant need for blood transfusion. According to the data from the Ministry of Health and Family Welfare, every year, 10,000 to 15,000 children are born with B-thalassemia major and make use of transfusion. The Health Ministry also highlighted that there are 42 million carriers of the thalassemia trait in India. Thalassemia trait carriers are those people who don’t have the disorder but carry a gene that can become a disorder in their offspring if their partner is a thalassemia carrier as well. See the below diagram to understand it.
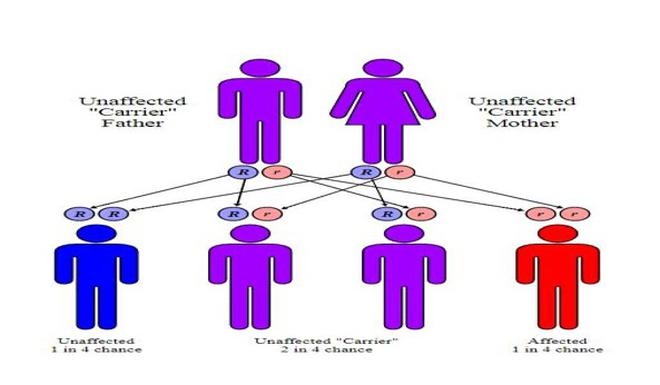
Any reader can be a thalassemia trait carrier and the only way to know is a blood test. Thalassemia is an easily preventable disorder and can be checked for in the nearest diagnostic centre. Thalassemia can also be detected in a neonatal screening test which allows people to make an informed choice for their future.
The Government of India has been working on thalassemia prevention and management. The National Health Mission has come up with guidelines for the prevention and management of hemoglobinopathies. The mission is to improve the care of Thalassemia and Sickle Cell Disease patients and reduce the prevalence of hemoglobinopathies through screening and awareness strategies. Community education and awareness programs, sustainable carrier screening programs, premarital and pre-conception screening, and extended family screening are all part of the strategy. For the management of the disorder, the goals of the public health strategy for thalassemia and sickle cell disease include providing optimal care through daycare facilities and safe blood, financial support for essential medicines, early diagnosis and intervention protocols, and community education. The strategy aims to improve treatment and management options and make them available through public health facilities.
Understanding patients with Thalassemia
Conversations about thalassemia for its management and prevention by the administration, thalassemia societies and caregivers of people with thalassemia have been rewarding to people with thalassemia like me. Access to quality disorder management and experienced medical professionals give a chance to people with thalassemia the to lead a better quality and a much more fulfilling life. Thalassemia was and still is considered as a pediatric disorder but that understanding has been left in the past when people with thalassemia had a life span of adolescence. Today, people with thalassemia are having long and fulfilling lives with proper management of the disorder and access to better healthcare. However, since the disorder is evolving and adult thalassemics are having different medical issues there is a need to update our medical curriculums and take a closer look at how the patterns of disorder change when patients reach adulthood. It is important to note that it doesn’t necessarily mean that every patient is reaching adulthood with a better quality of life.
Patients reaching and having healthy adulthood is a minority case still. A recent study conducted by the American Society of Hematology in India highlighted that only 50% of patients are able to survive at the age of 27 years. The numbers are worrying, and as I write this article it makes me terrified to think about my future as well but the numbers are hopeful as we have seen a much worse scenario. Healthcare advancements have shown us a quality long life is possible to achieve with access to management facilities such as safe blood transfusions and regular medicines.
However, the definition of quality life goes way beyond just survival for persons with disabilities. Access to healthcare provides an opportunity to maintain a longer healthier life but it doesn’t make life fulfilling in nature. In order to have a fulfilling life any individual should have access to quality education, livelihood and living a life free of stigma. Thalassemia impacts every segment of your life. Regular blood transfusions and medical procedures constantly impact education and work resulting in a lack of reasonable accommodations. People often deny believing that thalassemia is a disability or if it at all impacts us at a scale where our daily life is affected.
As a person with thalassemia, I have to undergo a transfusion every 15 days. The blood transfusion process takes about 4 to 6 hours depending on the units transfused. On average I’ve to get two units of RBCs transfused every 15 days. The number of units depends on a person’s weight and haemoglobin levels. The process is often a painful process which shoots up the iron levels severely and regular medication (approx 14 pills a day for me) is required to manage it. These pills have side effects on vision and bone density.
Accessing this level of healthcare services is not only cumbersome but also a heavy expense for families. The average money spent on thalassemia medication is around ₹15,000. Access to employment opportunities is a prerequisite for sustaining my health needs. However, there are myriad challenges faced by patients with thalassemia when it comes to employment like unavailability of flexible work options. Flexible work options allow people with disabilities to take care of their periodical medical procedures.
This write-up cannot exhaustively enlist issues faced by people with blood disorders in every sphere of life. However, I hope we can begin a conversation about a few of them. Thalassemia is a blood disorder but it is also a way of life for lakhs of us. Thalassemia advocacy needs to go beyond medical procedures. There are hundreds of young and brilliant people who are being devoid of opportunities at workplaces because employers are not sensitized enough to believe in us. Unfortunately, we have no official data or study on dropout rates or employment opportunities for thalassemia patients in the Indian context that can give us a clearer picture.
Thalassemia is not a simple disorder and it takes a village to manage it but it is possible. Parents and families become the foundation of this management and hence it is important to sensitize families about the disorder. Families have to believe in their children and also in their child’s dreams and hopes. All of those dreams, if they are not about unicorns and ponies, trust me are possible.







