
The disruption to cancer services during the pandemic has been a global phenomenon. In the UK, it has amplified structural failings in the delivery of cancer diagnosis and treatment that existed long before lockdown restrictions started in March 2020.
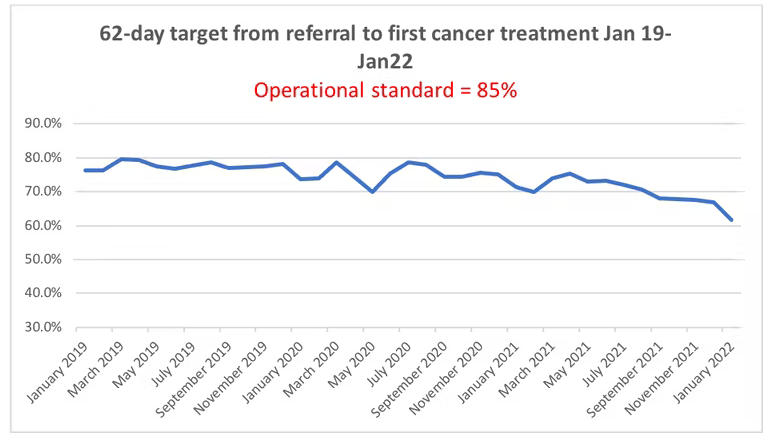
A report by Cancer Research UK (CRUK) in April 2019 showed that the UK had worse survival rates than many western countries due to inadequate early cancer detection and a lack of access to the best treatments. The report also acknowledged a shortage of cancer treatment specialists and that the target for treating 85 per cent of cancer patients within 62 days of an urgent GP referral had been missed every year since 2014.
By April 2020, it was evident that the NHS would not be in a strong position to cope with the increasing demand for cancer services at the end of lockdown. This is now reflected in the worst UK cancer waiting times on record. NHS England data confirms that in January 2022, only 61.8 per cent of patients started cancer treatment within 62 days of urgent referral (the target is 85 per cent), and 75 per cent of urgent cancer referrals were seen within two weeks (the target is 93 per cent).
There are already published reports of an increase in patients with later-stage cancers due to delays in diagnosis. Data from the NHS South East London Cancer Alliance confirmed a 3.9 per cent increase in people being diagnosed at an advanced stage of cancer (stages 3 and 4), with an overall 6.8 per cent increase in stage 4 cancers during this period. The greatest shifts were seen in lung (6.3 per cent), colorectal (5.4 per cent) and prostate cancer with a 3.8 per cent increase in stage 4 disease.
The failure to protect cancer services during lockdown, and the resultant delays to cancer diagnosis and treatment, will lead to worse survival. This will have a negative effect on the NHS Long-Term Plan (2019) to increase the number of patients diagnosed with early-stage cancer (stages 1 and 2) from 50 per cent to 75 per cent by 2028. With a 4 per cent shift to later-stage diagnosis during the first year of lockdown, and the probability that this will increase to 10 per cent over the two-year lockdown period, this target currently looks untenable.
In May 2021, a cross party cancer summit report was submitted to the UK government following input from a wide range of cancer specialists, professional cancer bodies and cancer charities. The report recommended ring-fenced cancer funding, with oversight by a government minister supported by an independent advisory group of cancer experts, to deliver a radical new cancer strategy.
The main strands of the report included recommendations to develop both short- and long-term workforce planning, invest in diagnostic and treatment equipment such as radiotherapy, overhaul the outdated IT infrastructure and digitise services where appropriate.
However, there has never been a better time for the NHS to review its cancer services, to develop a strategy that goes much further than simply focusing on reducing cancer waiting times, recruiting more cancer specialists and improving access to imaging and radiotherapy.
There is much benefit to be gained by focusing on the early part of the cancer journey through screening, diagnosis or treatment. Cancer prevention, personal risk assessment and risk reduction strategies should form a cornerstone of this cancer strategy while reviewing current national screening programmes, the management of urgent cancer referrals and access to optimal cancer treatment.
An ounce of prevention
According to CRUK, 38 per cent of UK cancer cases are preventable. Many risk factors for common cancers are already understood, but how many people know that obesity and alcohol are risk factors for both bowel and breast cancer, or that over 50 per cent of bowel cancer can be prevented? Greater education is therefore required to make these risk factors more widely known, with access to support to help people change their behaviour.
Cancer screening also contributes to cancer prevention, as well as early cancer detection. But NHS screening services need to be updated to consider personal rather than population risk and to address falling attendance rates.
By using family history, lifestyle risk scores and DNA tests that detect tiny genetic errors that increase the risk of a specific cancer, screening programmes that focus the NHS’s attention on those at higher personal risk of specific cancers can be developed. Urgent assessment of additional screening programmes for lung and prostate cancer should be considered, and at-home HPV testing for cervical cancer should be accelerated.
Any new cancer strategy will also require everyone to take responsibility for their own health and cancer risk. It should be the role of the government to provide the necessary education to allow people to understand their personal risk and to provide access to updated, streamlined screening and diagnostics that harness recent developments in science and technology. Without tackling all these structural issues, the UK will be unable to significantly improve national cancer survival rates.
Gordon Wishart is a visiting professor of cancer surgery at Anglia Ruskin University. This article first appeared on The Conversation.







