
A $24m question mark hangs over lowering the bowel cancer screening age
Newshub leaders’ debate host Paddy Gower motioned to the audience, where Aimee-Rose Yates was sitting.
“She’s got stage four terminal bowel cancer and she’s in her early 30s.”
READ MORE: * More gameshow than gamechanger * Debates pull in audience despite TV decline
About 1200 Kiwis die from bowel cancer every year, and, “they’re getting younger and younger”, Gower said. The minimum age of eligibility for screening sits at 60.
Yates’ question to the political leaders was: “Will either of you lower the age of screening and save the lives of Kiwis?”
National’s Christopher Luxon affirmed: “Yeah, I’d like to do that.”
Did Labour’s Chris Hipkins want to bring down the age as well? “Absolutely I do.”
Both leaders committed to matching Australia’s age of 50, or 45 if asked for.
Bowel Cancer New Zealand’s chair Stefan Corbett called the pledge from Luxon and Hipkins fantastic news which will mean fewer lives are lost to the “silent killer”.
(Right now, Te Whatu Ora/Health New Zealand’s priority is lowering the eligibility for Māori and Pasifika to 50, with an “evaluative implementation” underway in Waikato.)
Corbett’s charity expected the election winner to move quickly to lower the age for screening eligibility. That would be reasonable if the national bowel screening programme was well-staffed and working well in the public sector.
However, figures released to Newsroom show that, in this past financial year, Te Whatu Ora spent more than $24 million for patients from the public service to have 17,459 bowel procedures, like colonoscopies and colonographies, in the private sector.
The amount spent has progressively increased since 2017, when the programme started, with the Hutt Valley and Wairarapa district health boards. That year, the figure was $4.5 million.
Five years later, when Bay of Plenty was the last DHB to join the programme (just before it was disestablished with all other DHBs), a total of $73.5 million had been spent on private sector bowel procedures. (Almost three-quarters, or $54 million, was spent by three DHBs: Waitematā, Bay of Plenty, and Canterbury.)
Sarah Dalton, chief executive of the Association of Salaried Medical Specialists (ASMS) – the union for senior salaried doctors and dentists – says lowering the age of eligibility right now is unrealistic.
“It’s really easy, isn’t it, to say all these things that people are going to deliver or going to do, when it’s an election campaign, but there’s no real intention to look at health funding in a comprehensive way with any real understanding of what these undertakings mean.”
(Last month, ASMS released a report, Creeping Privatisation, which said a lack of investment in public health has led to a rapidly increasing dependency on private services. “In a world desperately short of health workers, Aotearoa New Zealand’s private health sector is inevitably poaching from an already over-stretched public hospital workforce.”)
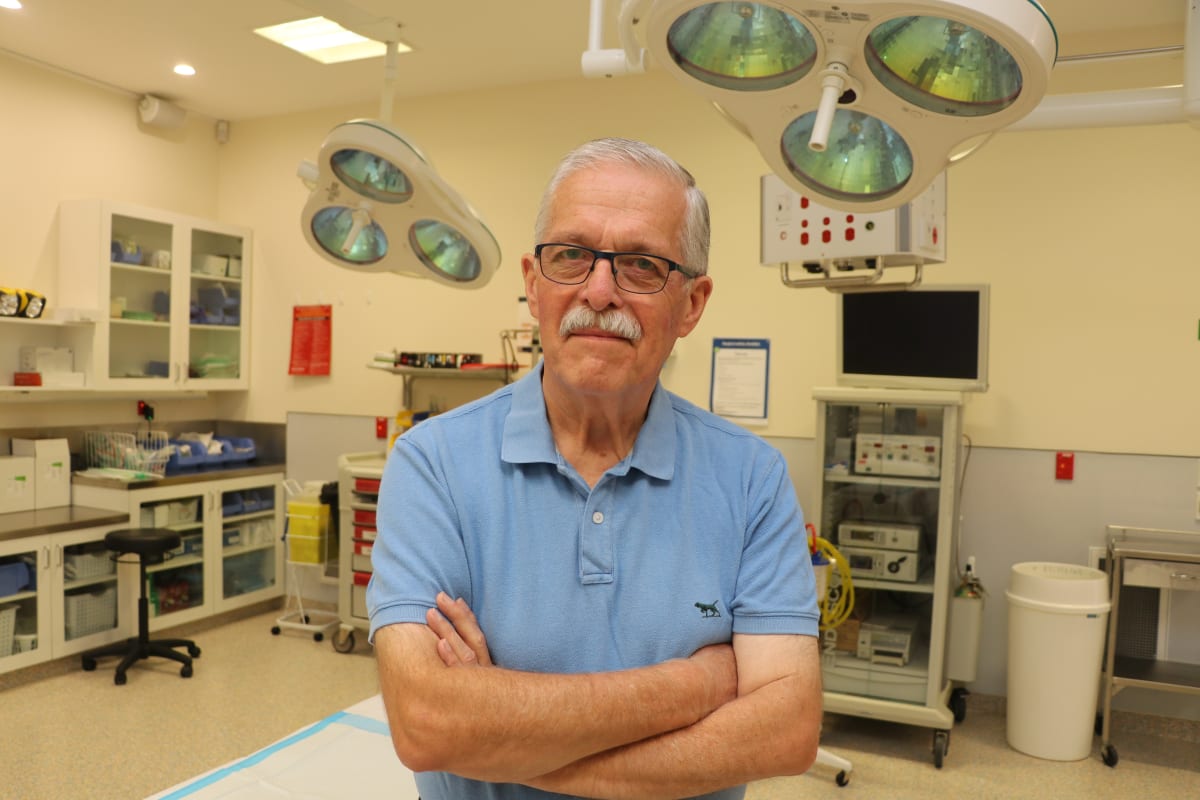
Meanwhile, Canterbury Charity Hospital co-founder Phil Bagshaw, whose hospital undertakes endoscopic procedures for symptomatic patients aged under 50 with rectal bleeding, says: “There's no way we can cope with that.”
Already, National and Labour have said any lowering of the age would have to be done in stages.
Newsroom asked the two main parties if they would commit to adequately resourcing endoscopy services before lowering the age.
“We have said that we will undertake a business case to explore lowering the age for bowel cancer screening,” National’s health spokesperson Shane Reti says. “Any hurdles will be identified by the business case.”
Reti said workforce was a key limiting factor for expanding endoscopy services, and National had already outlined plans to grow and retain health staff. His party supports improving frontline clinical capacity in the public health system.
Newsroom asked Labour why the national bowel screen programme wasn’t properly resourced as it was rolled out.
Health Minister Ayesha Verrall said: “As our health system continues to recover from the global pandemic, a number of services have had to be outsourced to make sure New Zealanders get the health services they need. We seek to grow public provision over time.”
However, blaming the pandemic ignores the millions of dollars being spent on external procedures every year before the programme started – including at least $7 million before 2017-18, almost entirely at Waitematā DHB, where a pilot project was established in 2012.
Verrall said Labour supports public services, first and foremost, as a matter of principle, and she noted health funding had increased by 45 percent since 2017.
Yet the cost of outsourced bowel procedures this past year cost $6.3 million in Waitematā, $4.9 million in Hauora a Toi Bay of Plenty, and $2.9 million in Waitaha Canterbury. In fact, external procedures cost more than $1 million in eight of 20 former DHB areas.
Verrall didn’t say if Labour would properly resource endoscopy services before lowering the eligibility age for screening.
Newsroom asked Labour and National if they knew how many extra staff or endoscopy units were required to adequately resource the screening programme throughout the country, but neither answered.
It’s worth turning the clock back to 2015, a year into the John Key government’s third term, when then Health Minister Jonathan Coleman laid out a timeline for the national bowel screening programme.
By then, more than 6000 people received a colonoscopy through the pilot project at Waitematā. Millions of dollars had been set aside in successive Budgets for extra colonoscopies.
(The procedure is a way to examine the bowels using a thin, flexible scope with a light and camera.)
Evaluations of the pilot were “positive”, Coleman said – not the best choice of words, perhaps.
In carefully couched language, the minister said he hoped to take a business case to Cabinet by the end of 2015. A “potential staged rollout” of the programme would happen from early 2017 – the year of the next election.
“Delivering better cancer services is a top priority for the Government,” Coleman said.
His 2015 press statement referred to the largest constraint of a potential national bowel screening programme – trained staff to do the colonoscopies. “Initiatives to strengthen the endoscopy workforce include increasing the number of gastroenterology trainees.”
That same year, Sarah Dalton started as an industrial officer, in the Auckland and Northland regions, at ASMS – the union of which she’s now in charge.
Dalton says the general rule of the now-defunct DHBs was to slightly understaff. If more people were needed, they would drag their feet, and write a business case.
She recalls union members working in gastroenterology services in Auckland saying they didn’t have enough people to do their current workload, let alone the additional work generated by a screening programme.
“These are all known issues.”
In June last year, Labour Minister Andrew Little said the programme – restricted to those aged 60-74 – had already detected 1400 cancers. “It could literally save your life.”
There was no mention of any workforce issues, or how many procedures were being outsourced.
Dalton, of ASMS, says, bluntly: “They said they’d be staffed but they never have been.”
Bagshaw says the procedures were being outsourced because public hospitals couldn’t cope with the extra work. He laments: “All of this was absolutely predictable.”
“They were robbing resources from symptomatic patients in order to do the screening.” – Canterbury Charity Hospital co-founder Phil Bagshaw
Long-time Newsroom readers will recall our 2021 story about long-standing problems with colonoscopy services in Otago and Southland.
Guidelines were used as “rationing tools” because of underfunding, said a report co-authored by Bagshaw, the Canterbury Charity Hospital co-founder. The allegation here is people who should have had a colonoscopy were refused.
The patients who weren’t declined colonoscopies (despite having symptoms of bowel cancer) faced, at times, long delays, with “adverse consequences”.
And it wasn’t just in the South Island.
Nationally, the decline rate of national gastroenterology referrals nationally was 22 percent in 2018 – as the national screening programme was being progressively rolled out, and well before Covid-19 hit.
As Bagshaw says of the screening programme, the more you look, the more you find. Since it was launched, more than 2000 cancers have been detected.
To be clear, no medical professional is saying screening is bad. But you need enough staff and endoscopy units to deal with both symptomatic patients – people with symptoms who are referred by a doctor or specialist – and the escalating need brought on by a screening programme.
Bagshaw believes Southern DHB’s symptomatic services weren’t adequately when it was given the go-ahead to join the screening programme.
“They were robbing resources from symptomatic patients in order to do the screening.”
Could this problem get worse because of the promises by Chrises Luxon and Hipkins?
Otago Daily Times columnist Elspeth McLean wrote last week: “It would be unethical to expand the programme to 50-year-olds if the system could not cope in a timely manner with the extra lab testing, colonoscopies, surgery and other treatments which might be needed.”
McLean makes another good point, which is that Australia’s trigger point for a referral – based on the amount of blood found in a faecal sample – is half that of New Zealand’s programme. This, it has been argued, is another rationing tool.
Given the situation now, what should be done?
Bagshaw says symptomatic patients should be the first to get procedures – and whatever’s left should be allocated to screening.
“If you want it to work, then we should have a massive increase in staff. God knows how many more endoscopic units would need to be built.”

Dalton, of ASMS, says little has been done by the public health system since Covid restrictions have eased to substantially take on more staff to undertake bowel procedures. But that corner of health isn’t alone.
“It’s just another dreary and depressing case study of our wider health system.”
This past Friday, Newsroom asked Te Whatu Ora a series of questions, including the latest published figures for: waiting times for symptomatic patients, declined referrals for endoscopy, and mortality rates for bowel cancer.
We were told a response wouldn’t be possible until close of business on Tuesday.
One of the country’s most prominent advocates for cancer patients is Southland’s Melissa Vining, whose late husband Blair was told, in late 2018, he had six-to-eight weeks to live – but an “urgent” appointment with an oncologist was eight-to-10 weeks away.
The Vinings were forced to pay for private treatment to prolong his life. (Blair died almost exactly four years ago.)
Melissa Vining tells Newsroom: “Due to the state of the health system, with long waits and staffing shortages, I see the future of New Zealand’s healthcare being delivered by a mix of private and public.
“Whilst I am in a position of privilege to have insurance, I know many everyday New Zealanders who are not, and my concern is that those with money or insurance will receive timely care and those without money – everyday Kiwis – will wait.
“Effectively, we will have a two-tier health system.”
Vining’s doing her bit to pick up the slack, though. She’s the driving force behind a new charity hospital in Invercargill, which is expected to open in the first half of next year.







