On September 11, samples sent to Calicut Medical College for testing were confirmed as Nipah virus. But only on September 20, after 323 samples were tested for the virus, did ICMR permit Kerala to use Truenat for Nipah testing. Even the belated permission came only after Kerala “strongly demanded” for Truenat during discussions with ICMR, Health Minister Veena George said during a press conference.
Truenat for Nipah virus testing was granted an emergency use authorisation (EAU) by the Indian regulator in September 2021 days after the third Nipah outbreak in Kerala. The EAU was based on validation of the Truenat test to detect the virus and the Trueprep AUTO lysis buffer (to inactivate the virus) by NIV Pune in 2018 in Kerala and external validation at the Institute of Epidemiology Disease Control and Research, Dhaka, Bangladesh. Both human and bat samples from Kerala were used for validating the test in 2018. In 2019, NIV installed Truenat at the Government Medical College, Ernakulam during the Nipah outbreak, and at two field sites in Punjab as part of the Nipah virus surveillance in bats. Of the 120 human clinical specimens and 25 samples from bats tested in 2019, Truenat correctly diagnosed all the positive and negative samples, except for one positive human sample.
As per a 2021 paper published in the Indian Journal of Medical Research, the sensitivity of Truenat was 97% and specificity was 100%. It was able to correctly diagnose Nipah even when other viruses were present. The efficacy of the Trueprep AUTO lysis buffer for inactivating Nipah virus prior to virus detection was also tested and found to be high. The “inactivation of Nipah virus was evident by the absence of Ct value”, notes the paper. A study was carried out at NIV in April 2020 using SARS-CoV-2 virus to evaluate the virus inactivating efficiency of both the lysis buffer and the Trueprep AUTO transport medium. The study, which is yet to be published but shared with The Hindu, found high virus inactivating efficiency by both the lysis buffer and the transport medium.
“The Truenat test for Nipah virus was already developed and ready as our idea is to work on diseases that have the potential to become a pandemic if not diagnosed early,” says Dr. Chandrasekhar Nair, Director and Chief Technology Officer at Molbio Diagnostics Pvt Limited.
Despite the validation as a point-of-care test by NIV and an EUA granted in September 2021, ICMR did not permit Kerala to use Truenat till September 2023. A senior scientist based in Kerala tells The Hindu that it is the Indian regulator and not the ICMR that is authorised to approve the use of Truenat for Nipah testing. With an EUA granted in 2021, States should have been free to use Truenat without any permission from ICMR, the scientist says.
BSL-2 facilities
“Truenat will be used for testing Nipah virus at five government medical colleges that have a BSL-2 facility with BSL-3 practices. Private medical colleges that have similar facilities will also be allowed to use Truenat,” says Hanish Mohammad, Principal Secretary (Health), Kerala.
“Testing for Nipah using Truenat is being considered only for hospital-based BSL-2 facilities and not in stand-alone labs,” says Dr. Aravind R, Head of Infectious Diseases, Government Medical College, Thiruvananthapuram. According to him, allowing only hospital-based BSL-2 facilities to test for Nipah is to discourage people from walking in to get tested at stand-alone labs. “The decision to test for Nipah should be taken by doctors, not patients. There should be a pretest probability of a patient being positive for Nipah,” says Dr. Aravind.
“The lysis buffer inactivates the virus and the risk is reduced maximally. There is no need for a BSL-2 lab for Nipah virus testing when Truenat is used,” says Dr. Raman Gangakhedkar, who was the Head Scientist of Epidemiology and Communicable Diseases at ICMR and a co-author of the 2021 paper.
Explaining why a BSL-2 facility is essential for testing Nipah virus, Dr. Rajiv Bahl, Director-General of ICMR says: “Even though in the diagnostic samples the virus may be inactivated by using lysis buffer, handling the initial samples before the addition to lysis buffer without strict containment measures may pose a risk of exposure to healthcare workers or any accidental environmental release if no proper decontamination is taken care of.”
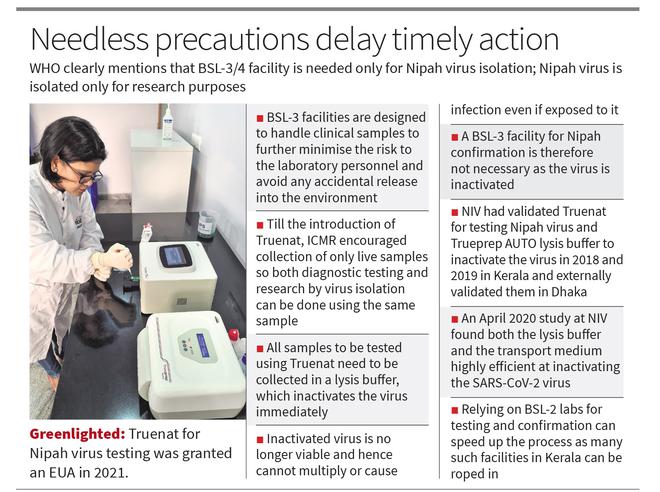
However, Dr. Nair of Molbio Diagnostics confirms to The Hindu that for Truenat, the virus is inactivated at the site of sample collection and not when the sample reaches the BSL-2 facility. Therefore, the inactivated virus is inert and non-infectious when the sample reaches the lab for testing. “The Trueprep AUTO transport media is a proprietary medium that has reagents to inactivate the virus. The transport media inactivates the virus while the lysis media in Trueprep AUTO completely breaks open the pathogens to release nucleic acids,” he explains. The April 2020 study at NIV found both the lysis buffer and the transport medium highly efficient at inactivating the SARS-CoV-2 virus.
Virus confirmation
ICMR and NIV are very clear that for an official confirmation, the sample must be tested only in a BSL-3/4 facility, says Mr. Mohammad. The insistence on a BSL-3 facility for virus confirmation is based on the 2021 government of India memorandum, he adds.
However, India’s rules on a BSL-3 facility for Nipah virus confirmation run counter to the WHO’s draft high priority diagnostics for Nipah. The WHO document mentions that Nipah can be confirmed by detection of the virus RNA or viral culture. For a reference laboratory setting, the “diagnostic options for confirmation can include laboratory NAT, NPT/POC NAT assays, virus isolation (if BSL-3/4 available), and serum neutralisation assays”. Of the diagnostic options for Nipah confirmation, WHO has included both near-patient testing (NPT) and point-of-care (POC) NAT testing; Truenat is a POC NAT test. The WHO also clearly mentions that BSL-3/4 facility is needed only when virus isolation is undertaken; isolation of viruses is only for research purposes.
“Viruses are sometimes cultured [for detection]. This used to be done a lot before nucleic acid-based amplification became available… Used much less now (and viral culture experts and lines are hardly available),” says microbiologist Dr. Gagandeep Kang, former professor at CMC Vellore. Dr. E. Sreekumar, Director of the Institute of Advanced Virology, Thiruvananthapuram says: “All labs in India, including the NIV’s, use only RT-PCR for Nipah diagnosis, be it for initial detection or confirmation. No other methods are used now.”
Usually, it is the same specimen that has been used for testing that is sent for virus confirmation, says Dr. Aravind. Dr. Sreekumar adds: “At present, ICMR encourages collection of only live samples so that they can do both diagnostic testing and research by virus isolation in the same sample. This [collection of live samples] prevents early detection as local labs are prevented from doing testing.”
But now, by default, all samples sent for Truenat testing are collected in a transport medium, which inactivates the virus at the site of sample collection. Since inactivated viruses are not viable, they cannot infect people; genomes can be sequenced using inactivated viruses. This makes a BSL-3 facility redundant for virus confirmation. Relying on BSL-2 labs for testing and confirmation can speed up the process as many such facilities in Kerala can be roped in.
Inactivated viruses are not only used for testing and genome sequencing but also for developing diagnostics, such as Truenat. “For any nucleic acid tests (NAT), the U.S. FDA accepts synthetic DNA. That is precisely how the U.S. and other countries developed COVID tests and the U.S. FDA authorised for emergency use even before outbreaks happened in those countries,” says Dr. Vinod Scaria, Senior Consultant at the Vishwanath Cancer Care Foundation, Bengaluru. “Even for drug discovery, live viruses are needed only for screening molecules and understanding the infection and immune processes. Even here, many scientists use pseudoviruses, which are better amenable and easier to use, for studying antibody escape.”
Responding to a question on why ICMR insists on a BSL-3 facility for Nipah virus confirmation despite the virus being already inactivated, Dr. Bahl, ICMR Director-General says: “BSL-3 facilities have specialised equipment and containment protocols to prevent the release of infectious materials. This is essential in case the virus is not fully inactivated or if there are any procedural errors during diagnosis.” But NIV had validated the Trueprep AUTO lysis buffer and the transport medium and found it to be really effective in inactivating the virus.