
A leading doctor and researcher says the COVID-19 pandemic has had an "awful" impact on the lifestyles of older people, who remain in a quandary about how much risk to take.
Four more Hunter people, three in their 80s and one in their 60s, joined the region's death toll on Sunday. Three were from Newcastle and one was from Singleton.
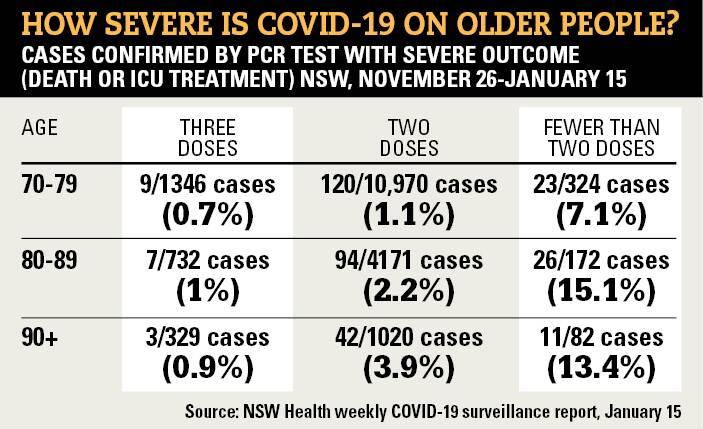
NSW Health figures show 2407 triple-vaccinated people aged over 70 had COVID-19 in the seven weeks to January 15 and 0.8 per cent of them died or ended up in intensive care.
The rate of serious outcomes was much higher, 10.4 per cent, for the 578 people in that age group who caught the virus but had not had two doses.
University of Newcastle laureate professor Nick Talley, the editor of the Medical Journal of Australia, said omicron case numbers were falling but it was unclear how much virus would be in the community when the current wave was over.
The virus had curtailed how older people lived for two years and he expected them to increasingly throw caution to the wind "whatever the advice is".
"It's been awful. I don't know what else to say," the John Hunter Hospital staff specialist said.
"It's a really difficult situation to be in, and it's a judgment call.
"I still think we should be trying to keep cases down to some extent with wearing masks and social distancing, some sensible things while we try to get more data to know what to do.
"I think just to let the vulnerable elderly die off at one in 100 or more isn't exactly the sign of a decent society."
NSW chief health officer Dr Kerry Chant said on Friday that case numbers would "taper off" but "the question is how low it gets and what our, sort of, baseline level of transmission in the community will be".
National Seniors Australia Newcastle branch secretary Sue Johns said some older people remained locked away at home while others were taking more risks.
"We have to start living. We have to start enjoying our lives," the 75-year-old said.
"We don't have unlimited time. We have to start not being fearful of each other. It's not good for our physical health, our mental health, our social wellbeing.
The Newcastle branch, which has about 70 members, cancelled all its events and meetings in the past two years except for two brief periods of relative freedom in 2020 and 2021.
The group met last week, and 30 to 40 members have put their names down to attend events in the coming months.
Ms Johns said most in the branch she had spoken to in the past fortnight "generally wanted to get on with life" but some were more cautious.
Many had missed seeing newborn grandchildren, holidays, birthday parties and social events.
"They were tired of living in this aura of fear," she said.
"They wanted to be responsible for themselves and make their own decisions.
"If they wanted to wear a mask, then fair enough. If they didn't, that was how they felt.
"There were a couple of members who thought our meeting should have been cancelled.
"A couple of people mentioned that there were people they knew who were just isolating, even though they didn't have to stay at home."
She said many older people did not feel as vulnerable as they were portrayed.
"We've probably reached that stage where we recognise our mortality. We recognise that we're all going to die at some stage and something is going to cause that death.
"It could be COVID. It could be influenza. I understand influenza deaths were up in their thousands before COVID came along."
Professor Talley said it was unclear how omicron would settle in the community and no magic bullet was in reach to protect older people, though omicron-specific vaccines were on the horizon.
"It's a real issue. I'm concerned about it. No one knows what the best approach is going to be. Is it going to be adding another dose, like Israel?
"All of those questions remain unanswered. There's no answer.
"It's a real quandary, and we won't know possibly until the end of the pandemic whether we've done the right things or not."
He said the omicron mortality rate was similar to the flu's and it was "not unreasonable" for triple-vaccinated older people to assess the COVID-19 risk as they would for flu.
"It's still a relatively low risk. One per cent in terms of severe outcomes is not that low, but it's relatively low.
"We used to have death rates that were not insignificant and hospitals would fill up each year with flu cases.
"You have to be careful of the analogy because it's not perfect, but that's kind of where we're at at the moment."
Ms Johns said media outlets were disseminating "constant fear" of the virus.
"After a while you have to turn it off and go, 'I'm just not listening to it anymore. I'm not going to take any notice of it.'
"I want to see the businesses up and going. I want to see hospitality back. I want to see jobs for young people.
"Everyone needs to be out there enjoying some things."
NSW recorded 28 deaths in the latest reporting period, but the number of people in hospital with COVID-19 fell again to 2321, down more than 400 in a week.
The number of COVID patients being treated in intensive care now stands at 147, down from 185 a week ago.
The HNEH health district has 53 COVID patients in hospital, including five in intensive care.
The district reported 936 positive tests in the 24 hours to 4pm on Saturday. NSW reported 7893 positive test results, the lowest count in 40 days.
Of the NSW fatalities, two were in their 40s, three were in their 60s, six people were in their 70s, 10 were in their 80s and seven were in their 90s.
A Port Stephens man in his 70s was among the 18 deaths reported in NSW on Saturday.
The health district's death toll stands at 78 since August.







