
Human reproduction is completely dependent on the healthy function of an underestimated but vital organ: the endometrium. This is the spongy tissue that lines the inner surface of the womb.
In the first half of the menstrual cycle, a healthy endometrium expands in response to the estrogen produced by a growing egg. The endometrium is then shed each month during menstruation.
Or, in the case of pregnancy, the endometrium accepts and nurtures the embryo.
So you’re trying to get pregnant. What happens?
When ovulation is triggered, the ovary starts to produce the hormones estrogen and progesterone. Progesterone causes the endometrial cells to prepare to accept an embryo, in a unique transition called “decidualisation”.
During decidualisation, endometrial cells display proteins that indicate it’s receptive for embryo attachment. After attachment, the junctions between endometrial cells loosen so an embryo can move beneath the endometrial surface.
Endometrial cells secrete substances that nurture the embryo, while immune cells protect the embryo and the endometrium while they move together and the placenta develops.
Read more: Health Check: how to get pregnant
The surface of the endometrium is covered by a shield of glycoproteins (proteins attached to sugars) which protects it from bacteria and viruses. This shield can also prevent an embryo from attaching to the lining.
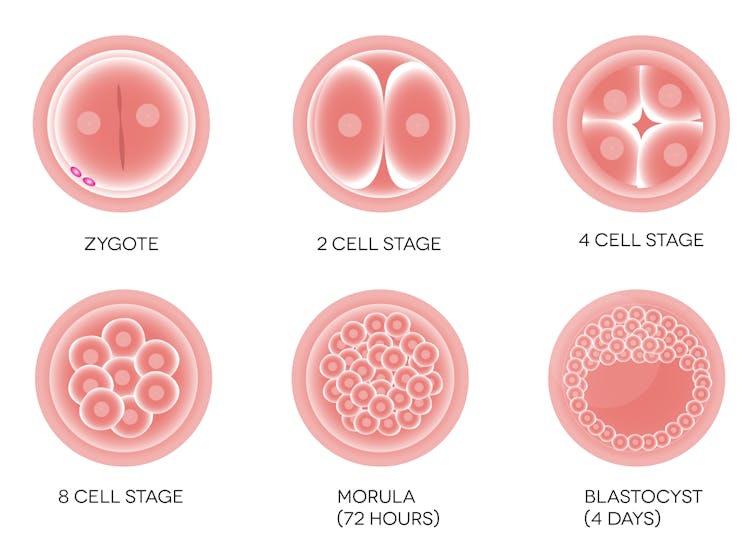
Progesterone helps to remove this glycoprotein shield about five days after ovulation. This is carefully timed so a fertilised egg will have developed into a blastocyst-stage embryo and be starting to hatch from its shell ready to interact with the exposed endometrial cells.
It prevents the body rejecting the father’s sperm
The endometrium must also retrain its immune cells to accept an embryo that contains the father’s foreign biological material, or “antigens”.
Tissues bearing these foreign antigens would usually provoke an immune rejection response, but the endometrium has adapted its immune response so an embryo can be accepted, and implant and grow, without rejection.
Although not essential for pregnancy, prior contact with the father’s semen primes the mother’s immune response and promotes acceptance of an embryo. Sexual activity enables paternal antigens, which are present in the fluid around sperm, to interact with the mother’s immune cells in the cervix and endometrium.
Read more: What's the point of sex? It's communication at a biological level
Paternal antigens are taken to lymph glands in the pelvic cavity where they are processed in a way that encourages the mother’s immune response to tolerate – not reject – these paternal antigens.
When paternal antigens on the embryo are next seen by the mother’s endometrial immune cells, they accept the embryo and nurture it. Implantation and placental development can then occur, maximising the chance of progression to a healthy pregnancy.
Then what happens?
For an embryo to grow beyond being a blastocyst, it must secure access to a robust blood supply. Oxygen and nutrients are sourced from the mother’s endometrium (called decidua in early pregnancy) during implantation via the placenta which is formed from outer cells of the embryo.
The process of implantation involves a complex sequence of cellular steps that must progress correctly for pregnancy to occur.
The endometrial tissues have to be reorganised so the blood vessels grow towards the embryo. These vessels then open up to allow blood to flow into blood-filled spaces (called lacunae) that bathe the surface of the placenta. This allows oxygen and nutrients to move from the mother’s to the fetus’s blood supply.
As these connections form, there can be minor bleeding a few days before a menstrual period is due. This is called “implantation bleeding”.
If any of these steps go awry, the embryo may fail to implant, there may be a brief interaction between the embryo and the endometrium that becomes disrupted (a “biochemical pregnancy” or very early miscarriage), or there may be implantation faults that cause a miscarriage some weeks later.
What can go wrong?
The events at implantation have consequences for the rest of the pregnancy.
Even minor defects in the embryo or endometrial interaction at implantation can increase the risk of common pregnancy conditions such as:
- preterm labour
- high blood pressure (preeclampsia)
- sub-optimal fetal growth
- premature delivery
- pregnancy loss.
What conditions affect the endometrium?
Inflammation is the hallmark of an unhealthy endometrium and contributes significantly to implantation disorders and miscarriage.
Endometritis (infection of the endometrium) and inflammatory fluid from blocked fallopian tubes (hydrosalpinx) can damage endometrial cells.
Dying and damaged cells attract immune cells that attack and engulf them. When damaged or dying cells are in the endometrium (decidua), the placenta doesn’t grow well and the pregnancy can be affected.

Endometriosis (endometrial tissue outside the uterus) and adenomyosis (endometrial tissue in the muscle of the uterus) also increase inflammation. In these conditions, endometrial cells in the wrong location grow and then die in response to cyclic menstrual cycle hormones. The immune system then has to be activated to clear the dead cells, creating an inflammatory environment.
Autoimmune conditions and metabolic disorders such as diabetes and insulin resistance also activate the immune system and create an inflammatory endometrial environment. These conditions have been linked to recurrent miscarriage.
How can you improve your endometrial health?
There are several things you can do to support a healthy endometrium.
First, manage the lifestyle factors that increase stress on cells and promote inflammation. This will decrease the chances of implantation problems and miscarriage.
Cutting down on smoking, marijuana, too much coffee or alcohol, and avoiding sugary and processed foods will make it easier for the endometrium to stay healthy.
For some women, the diagnosis and treatment of medical conditions that cause inflammation, such as diabetes and autoimmune problems, ensures treatments can start. Treating these conditions can reduce the risk of miscarriage and pregnancy complications.
Read more: Considering using IVF to have a baby? Here's what you need to know
Louise Hull is Professor and leader of the endometriosis and endometrium group at and at the Robinson Research Institute at the University of Adelaide. She works as a Fertility Specialist (FRANZCOG, CREI) and is also the Medical Director / Owner of Embrace Fertility, Adelaide. Louise has previously received funding from the Federal Government Grant for the EndoZone project and MRFF Funding for Imagendo. Louise Hull also works as a Staff Specialist Consultant at the Women's and Children's Hospital Adelaide
Sarah Robertson receives funding from the National Health and Medical Research Council of Australia, and the Australian Research Council.
This article was originally published on The Conversation. Read the original article.







