Sometimes there is a bleakly effective logic to underinvesting in public services. If they survive, then great, the money was saved. If they fail, then even better, because privatisation is here and ready to pick up the pieces. A classic example of this strategy is the NHS.
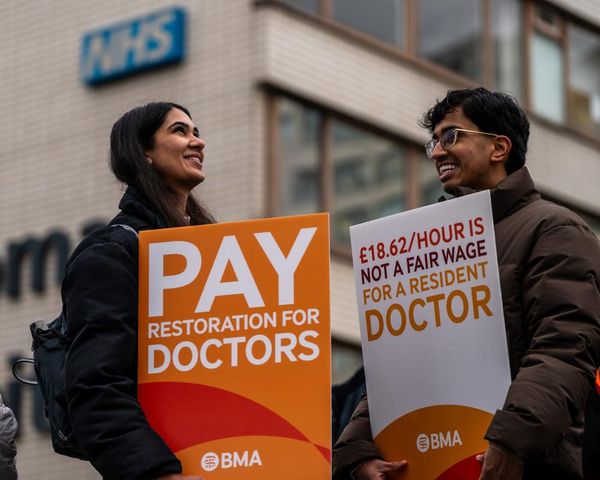
Junior doctors are working longer and harder, being paid next to nothing for it, and then blamed when things go wrong. There may soon be future strikes as their requests have not yet been met. Even though it is primarily about pay restoration, there is a wider context. They are now expected to put in extra shifts, compromise their career progression, and do work above their pay grade with no training or reward. This is by design.
Whenever the government reduces funding but maintains the service it is defunding, there is an undeclared expectation: the shortfall will be plugged by additional unpaid work and professional sacrifice. Staff are forced to crash course their training and dig deep into their moral and psychological reserves in order to make decisions they have not been adequately prepared for. The added salt in the wound is that the targets of patients’ distress are the staff right in front of them, not an abstract criminal history of a lack of investment.
This is also part of the design of underfunding, to shift responsibility on to those on the scene of the tattered service – slash and run, leaving the knife in the hands of those left behind. Our experiences with the NHS can happen at the sharp end of physical pain and emotional distress, and so the blame for its failures is understandably directed towards the institution and those who staff it: doctors who make mistakes or don’t show up, nurses who seem listless and unresponsive, or GPs who dispatch you after a five-minute consultation or cannot escalate your case quickly enough. Verbal and physical abuse of NHS staff is now a hazard of the job. They simply brace themselves before going to work.
And if you’re going to deny better conditions and pay for anyone, doctors are the easiest to justify. They are white collar, have high earning potential as their careers progress, and enjoy a professional prestige that makes it easy to target them as greedy or irresponsible – as the rightwing press has not wasted a moment in doing.
It is a testament to the enduring popularity of myths about the entitlement and poor work ethic of NHS staff, and striking workers in general, that just 54% support for the junior doctors’ strike is considered high. The government can still count on this bias, and the propaganda that sustains it, in its refusal to negotiate. The narrative focuses on the challenge that another strike will bring to a struggling system just so that doctors can get paid more at a time when everyone else is facing a cost of living crisis.
But it’s not about pay. It’s more existential than that. It’s about the limits of what humans can do when governments abdicate. What is asked of junior doctors now makes the entire practice and purpose of medicine questionable, let alone the viability of the NHS. A junior doctors’ strike is about commitment to a model of healthcare that, when properly resourced, provides free treatment to patients while also enabling doctors to receive the sort of wide-ranging medical training, research opportunities and academic specialisation support that they would never receive in the private sector.
As it stands, junior doctors pay hefty sums towards their own training and exams and they have to compete fiercely for a small number of senior positions. If they are from overseas, they have to pay huge, escalating sums for work permits and the residences of their dependents. Once junior doctors are consultants, they are too few in number, so have to lead, as much as is feasible, those junior doctors below them to do the work they cannot.
To expect junior doctors to continue like this is nothing short of holding them hostage to their choice of vocation and ambition to be the best doctors they can be. The government is asking them to take it or walk away. Increasingly, many across the NHS hierarchy are giving up. Almost 13,000 doctors gave up their medical licences last year, up almost 10% from the year before. They cite burnout, mental distress and impossible workloads. Nearly half of junior doctors are considering leaving the profession altogether.
Those who stay face a circular firing squad that compromises their ability to provide free, good quality healthcare and thwarts their ambition. Even an increase in junior staffing would be a drop in the ocean when there is no increase in bed capacity, no upgrades to administrative infrastructure, and no progression in a career that is founded on increasing specialisation. Junior doctors’ ability to continue to underwrite the government’s failures is not infinite, but the risk is that this state of affairs is normalised. The NHS has been under stress for so long that we have become desensitised to the toll of the crisis on both doctors and patients, and to the fact that it will, if nothing changes, inevitably reach a disastrous climax. I don’t know what that would look like, but I don’t want to find out.
Nesrine Malik is a Guardian columnist