
Years before Brenda Lyn Gavina had decided to devote herself to the exquisite field of pure mathematics, she was diagnosed with a condition affecting nearly 200 million women and girls worldwide: endometriosis.
“It was severe then, and I had to undergo open surgery,” Gavina, now a Ph.D. student in math at the University of the Philippines Diliman, tells Inverse.
Gavina didn’t keep her diagnosis to herself, however — a chance reunion with her college mathematics professor, Aurelio de los Reyes, led her to the idea that she could explore biological problems through the lens of mathematics, transforming organic issues into abstractions.
De los Reyes proposed a novel idea: Why not explore the reproductive system through mathematical modeling? Several years and one published study later, Gavina did just that, creating a mathematical model, alongside de los Reyes and other mathematicians in Korea, the U.S., and Denmark, of the menstrual cycle that found common contraceptives could reduce their hormone dosage by 92 percent and still be effective at suppressing ovulation (the process by which a mature egg is released from the ovary).
The findings, published this month in the journal PLOS Computational Biology, aim to use a mathematical framework called optimal control theory to lend valuable insights into better hormone-based birth control formulations and scheduling, potentially leading to more effective and safer methods of contraception down the road.
Math meets biology
In the simplest terms, the optimal control theory seeks to find the best possible way to control a system over time so as to minimize cost while also satisfying the system’s constraints.
For example, imagine you’re a time-weathered captain navigating a ship through stormy seas to reach your desired destination. The ship is the system being controlled, the destination is the desired outcome, and you, the captain, are the control algorithm tasked with optimizing the ship’s course and speed to reach the destination as quickly and efficiently as possible, avoiding obstacles like a fierce storm or icebergs (hello, Titanic) and minimizing costs like energy consumption.
The origins of optimal control theory can be traced back to the late 18th and early 19th centuries, and it's been worked on and perfected ever since. Today, optimal control theory has been applied in almost every aspect of science and technology, from aerospace engineering and economics to biology and medicine.
“It [was] in the late 50s or 60s when people started looking at what if we apply this optimal control theory in a biological model,” de los Reyes tells Inverse. “It’s been applied to cancer, diabetes, HIV, tuberculosis, and even infectious diseases like dengue and malaria.”
Transforming the menstrual cycle into math
Medicine, perhaps, perfectly encapsulates the goal of optimal control theory — in treating disease or illness, it’s all about getting just the right dose of a therapy or drug while paring down any side effects an individual may experience.
In the case of contraceptives, Gavina, de los Reyes, and their colleagues needed a mathematical model of the menstrual cycle (aka the system). It’s a bit more complicated than it sounds since what someone experiences as pain, menstrual bleeding, or mood swings belies what’s going on under the hood — the complex interplay of hormones produced by several organs in the body.
Before we go any further, here’s a sex education 101 recap: As we’re all (hopefully) aware, a menstrual cycle is a natural, monthly process divided into several phases marking different physiological changes in the reproductive system. Overall, the end goal is to get the body ready for pregnancy once the egg, released during ovulation, is fertilized, and if not, scrap everything entirely (i.e., a period) and set up a clean slate for the next month.
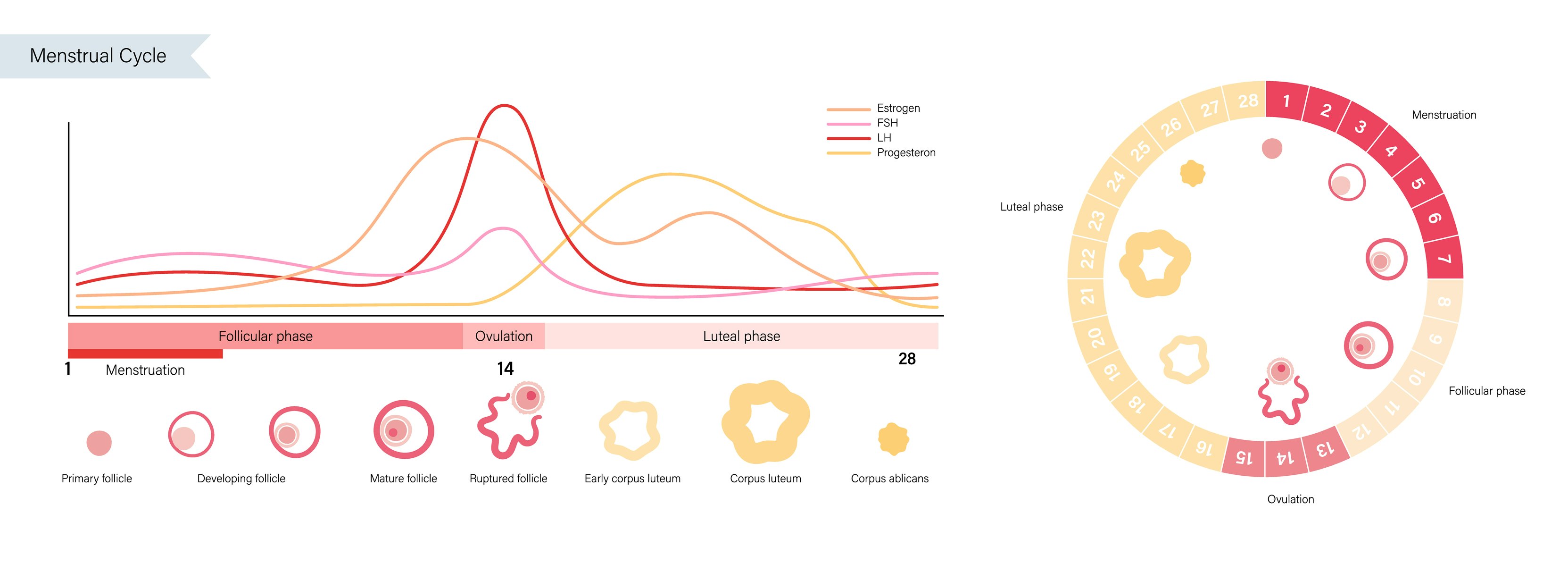
At the beginning of each menstrual cycle, the hypothalamus (an almond-sized region in the brain near the brainstem) releases a hormone called gonadotropin-releasing hormone (or GnRH), which signals a pea-sized gland just below it, the pituitary gland, to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These two hormones travel to the ovaries, where they encourage the growth and development of the eggs.
There are several other hormones that play really important roles in regulating the menstrual cycle, such as estrogen and progesterone. Imbalances in these two hormones can lead to menstrual irregularities and other reproductive health issues like endometriosis, polycystic ovarian syndrome, and infertility, to name a few.
Taking all these hormones (and another one called inhibin A, which regulates FSH) into account, the mathematicians constructed a menstrual cycle model based on data from 23 normally menstruating between the ages of 20 and 34 years whose cycles were, on average, 28 days long. (Gavina says this wasn’t data the researchers directly collected but extracted from a past study dating back to the late 1990s.)
This mathematical menstrual cycle model, Gavina and de los Reyes say, was able to accurately predict the expected changes in hormone levels throughout a normal menstrual cycle. When they included the effect of estrogen and progesterone from hormonal contraceptives, they found most contraceptives could make do with a lower dosage — 92 percent reduction for estrogen-only therapies, 43 percent for progesterone-only — while still preventing ovulation.
Through their mathematical simulations, the researchers also discovered there might be an optimal time to deliver an estrogen-only contraceptive, theoretically during the middle of the menstrual cycle or the mid-follicular phase.
Going back to the chalkboard
While the mathematical effort to make hormone-based birth control more tolerable without losing effectiveness is innovative, it’s nowhere near being clinically translatable, Elizabeth Deans, assistant professor of obstetrics and gynecology at the Duke University School of Medicine, who was not involved in the study, tells Inverse.
“I’m glad that someone is looking into this from more of a mathematical modeling perspective and not so much from a clinical perspective,” she says. “But they’re using a model based on 23 women [who] are aged typically younger, and there’s not a lot of other clinical information about them. That was some of my initial concern about using data from women with regular menstrual cycles, but what does that mean in terms of their [body mass index] or other medications [they could be on]?”
Alison Edelman, professor of obstetrics and gynecology and the division director of Complex Family Planning at Oregon Health and Science University, agrees and adds that the menstrual cycle model doesn’t appear to take into account how a hormone-based birth control interacts with the body once it gets inside, what’s called pharmacokinetics.
“A little bit of a fatal flaw for me as a clinician is that it doesn’t take into account the pharmacokinetics aspect,” Edelman, who wasn’t involved in the study, tells Inverse. “[The researchers] aren’t taking into account how synthetic hormones are absorbed, metabolized, and excreted. That’s a big deal for contraceptive development where we do these dose-finding studies to see what’s the balance of the lowest dose you can go that gives you the contraceptive effect you’re looking for [while] also balancing risk and side effects.”
The model is also built around optimizing hormone dosages for suppressing ovulation, which isn’t entirely the purpose of hormone-based birth control, Michelle Roach, assistant professor of clinical obstetrics and gynecology at Vanderbilt University Medical Center, who also wasn’t involved in the current study, tells Inverse.
“The whole concept to specifically suppress ovulation [with] lower doses of hormones is definitely interesting, but I think it's a little limited,” says Roach. “Birth control prevents pregnancy, suppressing ovulation is definitely of [those means]. But there are things that birth control does [such as] affecting the lining of the uterus, thickening cervical mucus, and decreasing the motility of the fallopian tubes.”
It’s important to note most hormone-based birth control currently on the market are already a low dose, says Deans and Edelman, and that there’s no such thing as a standalone estrogen contraceptive due to potential side effects such as blood clots, stroke, and cardiovascular conditions, particularly in women who smoke or have other risk factors. (Hence, why most common contraceptives contain progestin — synthetic progesterone — as the main contraceptive driver with a little help from estrogen.)
Deans, Edelman, and Roach say the idea of taking a contraceptive at an optimal time during the cycle is intriguing but is something that we sort of already do with emergency contraception, like Plan B, and also doesn’t guarantee to suppress ovulation entirely — instead, you might just be pushing it for later in your cycle. It also would be a difficult approach for individuals on hormone-based birth control to have to remember to take a pill on a certain day, throwing in an extra risk of missing a dose and reducing patient adherence.
“People now are tracking their cycles and have a lot more self-awareness around their cycles with the femtech that’s happening,” says Edelman. “But if you don’t have a regular cycle, which a lot of people don’t have, or you use something mid follicular phase or mid cycle, then your next cycles are not so regular, and it would be hard to know when to take [a hormone-based birth control].”
Both Gavina and de los Reyes acknowledge their mathematical menstrual model needs a lot more finetuning before it could ever be ready for clinical use.
“We have to emphasize that, like in a lot of modeling studies, we’re introducing simplified assumptions,” says Gavina. “It’s an ideal situation, so we have to be very careful in interpreting [the results] because what we have presented is not directly translatable to the clinical setting.”
The mathematicians do hope their research could help healthcare providers gain better insights into optimizing contraceptive dosing for conditions like endometriosis or polycystic ovarian syndrome, both of which are treated with hormonal birth control. More futuristically, perhaps their equations could even one day power wearables or “smart” birth control devices that sense changes in the menstrual cycle through specific biomarkers obtained through blood or a proxy, say, circadian rhythms to deliver just the rise amount of synthetic hormones a person needs.
A period tracking wearable taking care of all your birth control needs? Can we get a “Future now, please?”







