When a person is diagnosed with depression, they are typically guided toward therapy, medication, or a combination of the two. However, roughly 30 percent of these individuals don’t feel better after taking antidepressants alone, and while the demand for therapy is increasing many people who experience depression still do not seek help.
The scientists behind a new study argue this demonstrates why we need more accessible and non-stigmatizing therapies for people with major depressive disorder. Their research suggests a novel tool that can help spur relief is already on shelves in grocery stores and pharmacies across the country: probiotics.
According to research published in the journal Traditional Psychiatry, people who pair their antidepressants with probiotics experience a greater improvement in depressive symptoms compared to people who only take antidepressants. This study adds to a growing list of findings that point to a critical link between gut health and mental health.
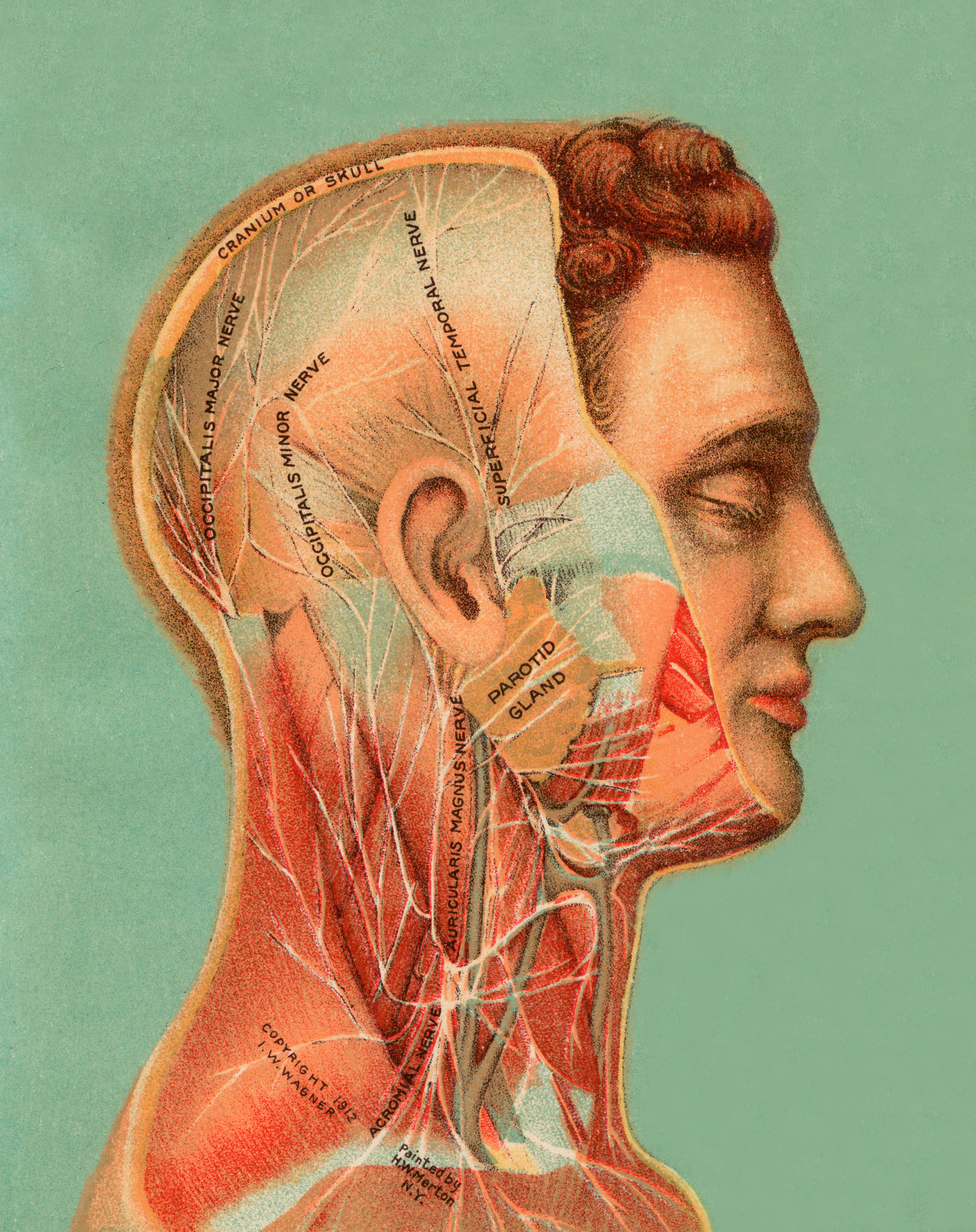
Antidepressants alter neurotransmitter activity in the brain. Probiotics, meanwhile, are beneficial bacteria that exist naturally in some fermented foods, like kimchi, and in pill and powder form. Early evidence suggests probiotics can help with mood and anxiety disorders because they influence the gut-brain axis, the two-way relationship between the brain and digestive tract.
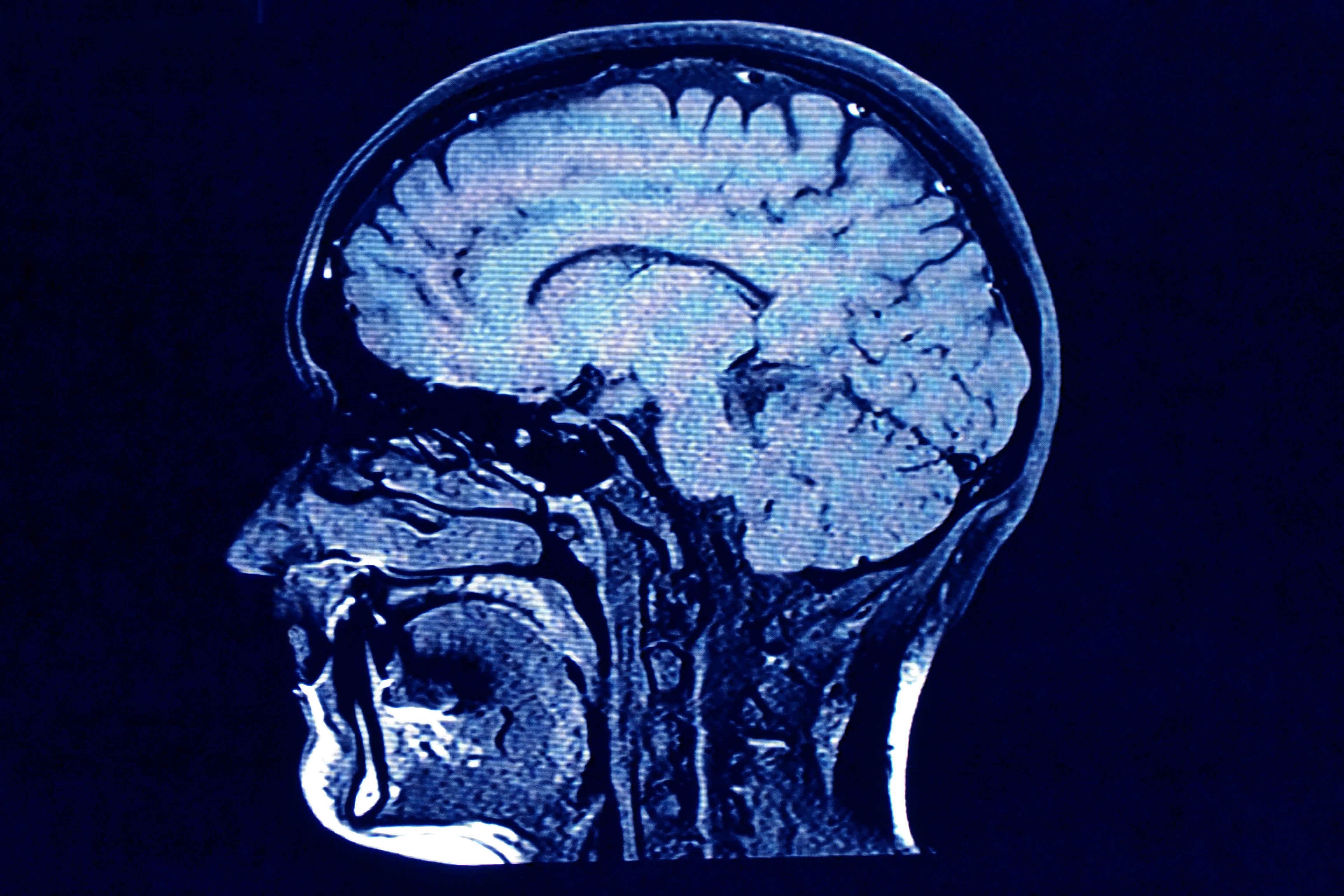
Brains scans of the study participants also revealed that the group who took probiotics experienced a beneficial change in the parts of the brain related to emotional processing. This study is viewed as the first to explore both how probiotics can change bacteria in the gut along with brain structure and function.
How probiotics can influence mood

To examine the effect of probiotics on depression, scientists recruited study participants already receiving medical help for depression. Within this group, 21 participants added probiotics to their treatment alongside antidepressants, while 26 received a placebo pill. The probiotic is called Vivomixx, which contains eight strains of live bacteria.
“As there is still no clear evidence which specific bacteria improves depressive symptoms, we decided to use a probiotic supplement that is easily accessible and thus easy to implement in clinical practice,” the study team writes. “To the best of our knowledge, no previous study investigating effects on depressive symptoms used such a high dosage.”
The study period was four weeks and the participants were evaluated before, during, and after the intervention. They completed a battery of tests, including stool sampling, brain imaging, and assessments of depression.
While all study participants experienced an improvement in mood because everyone was using antidepressants, the participants who were also taking probiotics experienced an even more significant change in mood.
They experienced some physical changes, too. For example, the scientists found that probiotics increased the abundance of bacteria belonging to the genus Lactobacillus. Earlier studies on animals also found an association between this type of bacteria and improved immune tolerance alongside beneficial effects on anxiety and depression.
The study team also took brain scans of the participants as they looked at images of neutral or fearful faces. During this type of experiment, the brains of people people with depression tend to perceive neutral faces as emotionally negative faces. However, in this case, the group that received probiotics was more likely to perceive neutral faces as neutral. Brain scans reflected a change in brain activity.
However, the makeup of the intestinal bacteria within the study group’s guts returned to normal after four weeks, losing much of the diversity thought to help mental health. This suggests to the study team that four weeks of a probiotic supplement might not be long enough to create lasting change and that future studies should test whether or not that’s true.
What is the gut-brain axis?
The physical and chemical connections between the gut and brain are due to what’s known as the gut-brain axis. This link flows in both directions and involves the autonomic nervous system, the enteric nervous system, the neuroendocrine system, and the immune system.
The gut-brain axis is why many scientists think the gut microbiome can influence mental health. There are 100 trillion microorganisms in the gut — a mixture of bacteria, viruses, fungi, and protozoa. Collectively they are known as the microbiome.
While more research is needed to know exactly why certain microorganisms are especially helpful, studies suggest a “gut-based approach” can help support emotional well-being. However, supplements like probiotics should be viewed as just one tool in the mental health toolbox. The authors behind the new study stress that probiotics should not be used as the only treatment for depression.
For now, talk therapy, exercise, and medications are the most effective and established ways to help ease depressive symptoms. But probiotics are an intriguing add-on, with increasing studies supporting their effectiveness.

.jpg?w=600)





