
Around 60,000 NHS staff members have post-traumatic stress after working through the Covid-19 pandemic, new research suggests.
Nine out of 10 health workers say it will take them years to recover from the ordeal and one in four had lost a colleague to coronavirus, according to NHS Charities Together
The charity, NHS staff and mental health experts are now calling for more support from the health service and UK government to support those struggling in the aftermath of the pandemic.
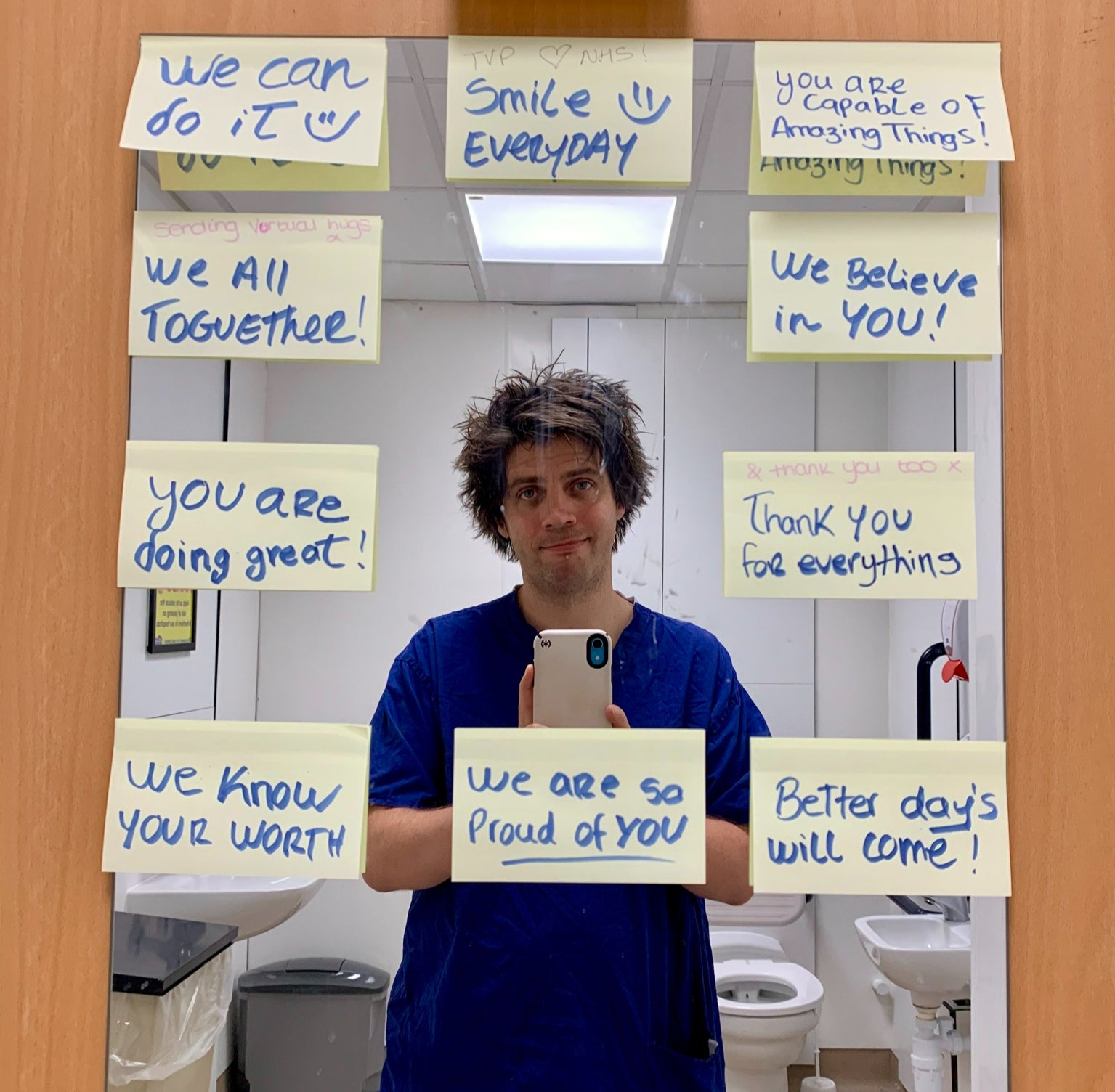
“I think it’s quite clear there hasn’t been enough support to help NHS workers recover from their experiences during the pandemic. As a result, a lot of people are feeling incredibly jaded,” said Dr Ed Patrick, an NHS anaesthetist who worked in a Covid-19 intensive care unit from the beginning of the pandemic.
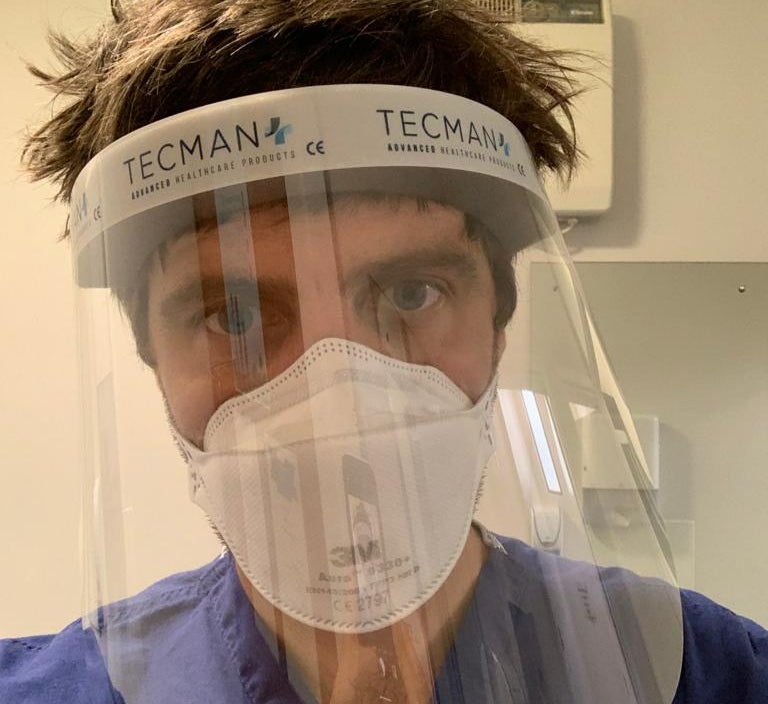
On his experiences of working on the front lines of the health service, Dr Patrick said: “Like everyone else in the world, we lost our outlets for release. Everything was shut down and for NHS workers, our lives just became the hospital.
“For me personally, it wasn’t until after the pandemic eased that I realised what I’d just gone through.”
He described the long and gruelling hours and the emotional burden of working at the height of the pandemic: “We all had an overwhelming feeling of powerlessness. There was also a deep sadness because everything you would normally do to help patients just wasn’t working.
“Usually if someone’s oxygen levels are low, you give them oxygen, and then their oxygen comes up. That just wasn’t happening in the Covid ICU.”
Dr Gauhar Sheikh, an anaesthetics doctor who was working for the NHS in Edinburgh at the time, described the difficulties she experienced on the frontline of the health service.

“Working in the pandemic in intensive care was quite an eye-opener,” she said. “I was part of the teams that needed to bring severely unwell patients to intensive care and escalate their plans. Some needed to be put to sleep and on a ventilator. Some made it and some didn’t. You remember each one.
“The biggest impact for me was not being able to see my elderly granddad in his last year of life and my new niece in her first year as much as I would have liked to,” Dr Sheikh continued. “I kept that distance on the grounds of health and the fact that I was working with Covid-19 patients directly.”
Both doctors are unsurprised by the rise of mental health issues, including PTS, amongst NHS workers and are calling for more support for them post-pandemic.
Dr Sheikh said she wanted more compassion for and understanding of what medical staff have face on the frontlines and Dr Patrick said there needed to be much more training and jobs available in the NHS to those who want them.
“It’s clear we need more doctors and nurses,” he said, “and because we don’t have these extra staff right now, NHS workers are getting burned out and it makes the system unappealing to work in.
“It’s sad because these people love their jobs, I love my job. But the reality is we’ve all been through a very traumatic time. There needs to be a way back for the NHS as a service and the people who work so hard to provide it. The NHS is the sum of its workers and those workers are asking for support.”
Dr Rhianna McClymont, lead GP at the medical app Livi, said: “Many frontline workers were exposed, and are still exposed, to death and dying at a scale few will have experienced previously, while being at risk of dying themselves.
“This could have a significant impact on them, and some are experiencing symptoms of PTSD, particularly around reliving traumatic events through flashbacks,” she added.
“The pandemic may have exacerbated their [pre-existing mental health] conditions and made it harder to treat. This is important because it should inform how their treatment is conducted in future,” Dr McClymont said.
Ellie Orton OBE, Chief Executive at NHS Charities Together, detailed how their charity is helping staff cope with their post-pandemic mental health. She said: “The NHS can’t face every challenge alone, and as the national, independent charity caring for the NHS we are proud to have funded hundreds of incredible projects supporting staff, patients and communities alike.
“We’re at the start of a long journey to recovery and there is always more that can be done – but we can only do it together.”
Ms Orton shared that the charity is inviting the public to support the NHS by joining its annual NHS Big Tea on Tuesday 5th July - the anniversary of the health service’s beginnings.
“Taking place on the NHS’ birthday, we’re inviting everyone to join in with the nation’s biggest tea break and raise a mug – and vital funds – for the incredible people of the NHS.
“They have done so much for us over the last two years and continue to give their all in the most challenging circumstances. By getting behind the NHS Big Tea you can make an important difference to staff wellbeing, and help the health service go further for all of us.”
Last year, the event raised £500,000.
An NHS spokesperson said: “Staff are the lifeblood of the NHS, which is why, in response to the pressure of the pandemic, we have strengthened the mental health support offered to them to make sure they get rapid access to assessment and evidence-based mental health services and support.
“This includes 40 local staff mental health and wellbeing hubs across the country, which provide proactive outreach and clinical assessment and a continued focus within NHS organisations on staff health and wellbeing.”
This article was amended on 17 May 2022. It previously referred inaccurately to post-traumatic stress disorder, but should have referred to post-traumatic stress.



!["[T]he First and Fifth Amendments Require ICE to Provide Information About the Whereabouts of a Detained Person"](https://images.inkl.com/s3/publisher/cover/212/reason-cover.png?w=600)



