Our society seems to have accepted that gaining weight is an inevitable consequence of growing up in a place with easy access to calories and where physical activity plays a declining role in our professional and private lives. Aging just makes weight loss even more difficult.
In the short term, the consequences of excess weight seem remote or unimportant; a problem of aesthetics, a minor limitation in mobility. But it may eventually lead to higher rates of diabetes and heart disease, and present a significant challenge for enjoying an active lifestyle.
My own work and that of my collaborators here and in the U.K. shows that obesity is more than just some more fat under the skin – it is a true modification of our metabolism. It alters the way we process nutrients and modifies the chemical reactions that sustain our existence. Our most recent work, published in Cell Metabolism, examined the consequences of obesity on our metabolism. My colleagues and I undertook this project because we recognized that there are many types of obesity – each one has different consequences for each person’s health. This is what we call disease “heterogeneity.” If we understand heterogeneity, we can personalize obesity treatments, hopefully with more success.
My obesity, my metabolome
We are a team of researchers with different backgrounds including medicine, technology and the analysis of complex data. We studied close to 2,500 obese people with two powerful new technologies: We sequenced the entire genome of each study participant, and we analyzed more than 1,000 blood chemicals, or metabolites. This collection of metabolites is what we now call the “metabolome” and includes well-known compounds such as glucose and uric acid, as well as tongue twisters such as 1-stearoyl-2-dihomo-linolenoyl-GPC.
We included the genome analysis to understand how an individual’s genes predisposes him or her to obesity. We chose the metabolome to capture in real time the impact of having excess weight. Many of the study participants were followed for more than 10 years; this enabled the assessment of long-term consequences of our observations.
The surprising and disturbing news is that the levels of many hundreds of unique metabolites are affected by changes in weight. Some of these changes were expected: Fats or lipids – including cholesterol – rise rapidly with increasing weight. However, we also observed changes for other types of metabolites and body processes: protein and carbohydrate metabolism, energy production and hormone concentrations.
The overall picture was that weight dramatically perturbs the body’s metabolism. The good news is that the alterations can be reversed with weigh loss.
The healthy obese and the unhealthy skinny
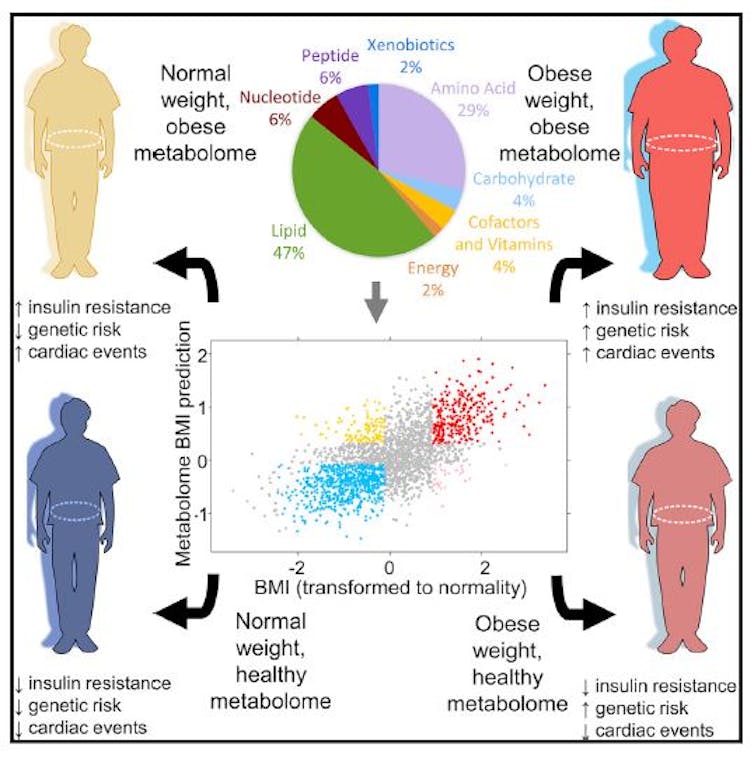
A second and fundamental observation was that the metabolic alterations carried more health consequences than the mere physical aspect: Some of the participants had what we labeled as an “obese” metabolome despite having a normal weight. On the other hand, some obese individuals had a pretty normal metabolome that was similar to those individuals with a healthy body mass index.
It is not clear to us how an obese person could have a normal metabolome. We do not know whether it is their genes or environment that are responsible for keeping this group of individuals more healthy. That will take more research to figure out.
Because we had medical information at the time that the metabolic analyses were performed and we had long-term follow up data, we could see the consequences of abnormal metabolism.
Those obese individuals who suffered the greatest deregulation of the metabolism developed diabetes, heart disease and hypertension. These same participants were also the ones that accumulated fat tissue inside the abdomen and in the liver – the “bad” locations – as opposed to just adding it under the skin of the waist or buttocks. Thus, physical obesity was important – but how the excess weight uniquely affected the inner workings of each individual was a more accurate measure of overall health.
Metabolome report may say more than your BMI
It may be tempting to think of obesity as the consequence of genes – inherited from our parents. It is true, but the impact of our genes pales in comparison to the overwhelming impact of high caloric intake and sedentary lives.
There was one exception. We identified a few very obese individuals who had changes in a gene that controls appetite – the so-called melanocortin-4 receptor (MC4R). These patients had a genetic mutation that made them permanently hungry and led them to eat more than they needed. There is great hope that this particular type of obesity will be soon treated with specific drugs. As expected, this form of obesity severely disrupted the metabolism of the affected person.
We see all the time that science provides new understanding on important health problems that seems to fade once the news cycle is over. But after the hype comes the incubation of new strategies that may eventually find their place in medical practice.
Specific to research in obesity, I believe that bringing attention to the important changes in the metabolism provides a sense of urgency to the field. This work also provides a new way to measure the harmful impacts of obesity and to screen populations to identify those who could benefit from participation in clinical trials of new drugs. This includes individuals who are skinny and have an unhealthy metabolome, but are unaware of their state of health and would benefit from early intervention.
Amalio Telenti was a previous employee and consultant of Human Longevity Inc.
This article was originally published on The Conversation. Read the original article.







