A vial of human serum, an ice box and an illegal flight: How an Australian doctor saved millions of babies' lives.
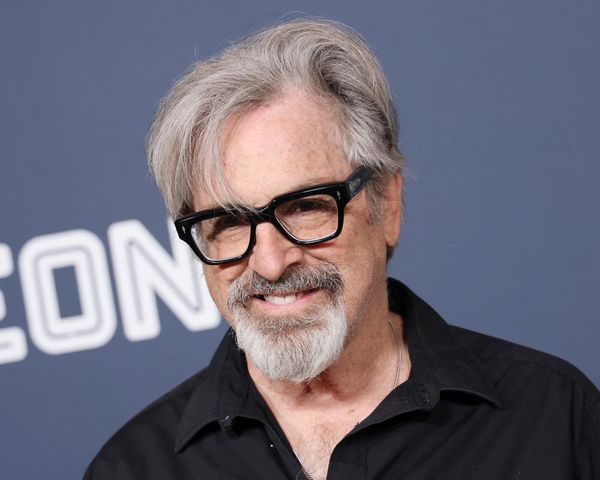
John Gorman is probably the most famous Australian you've never heard of.
His groundbreaking medical research to treat a blood disease has since saved millions of babies' lives around the world.
"It makes John Gorman one of the unsung heroes of Australian medical science," University of Melbourne deputy vice-chancellor and immunologist Jim McCluskey says.
"He's up there with Fiona Stanley, Gus Nossal, Peter Doherty, the titans of Australian medicine, Barry Marshall. He should have got a Nobel [Prize] but didn't."
John Gorman's path to medical pioneer began with an unquenchable curiosity and an instinct for adventure.
"My dad was the one [who] inspired me, more than anything. He was very interested in science and, even as a kid, I was into all kinds of scientific ideas," he told the ABC from his Californian home.
After completing his medical studies at Melbourne University and St Vincent's Hospital, Gorman set off overseas in 1955 with three great mates — also doctors — John Hamilton, Hubert de Castella and Sam Breen.
Setting sail on the SS Orcades, they travelled through Europe and then on to New York.
"I was interested at that time in becoming a surgeon. So I had the idea of going to America and then to England," Gorman says.
"We had a wonderful trip to New York. We got off the Orcades in Naples and then we rented a car and we drove all the way and ended up in London in time for Wimbledon. It was a fantastic trip."
He had a stint working in paediatrics at a hospital in the South Bronx before landing a job at the prestigious Columbia Presbyterian Hospital in New York as a resident medic in blood banking and laboratory medicine.
"As soon as I got into the blood bank, I knew that was for me," Gorman says.
"I was happy to get away from patients and, of course, one of the things that I got away from was the responsibility.
"You know, we had two children die that year, right in front of me. It was, it was … I didn't need that."
His time in paediatrics, both in Australia and the US, had made him familiar with Rh disease, for which there was no cure.
"At one point, 10 per cent of the neonatal deaths in Melbourne were caused by Rh disease," Gorman says.
"And the thing about Rh disease was, it's a silent killer. The mother feels perfectly good and then, all of a sudden, she's got a stillbirth."
Rh disease occurs when a mother's blood is incompatible with her unborn child's Rhesus, or Rh factor, which indicates the presence of the Rh-D protein in the red blood cells.
Having the Rh factor means you have a positive blood type, and if your blood does not have the Rh-D protein, you are negative. For example, 0+ means your blood has the Rh-D protein, A- means it doesn't.
About 85 per cent of babies are Rh-positive, while 15 per cent of mothers are Rh-negative.
"When you have that combination, the baby's red cells cross the placenta into the mother's circulation, and they start an antibody to Rh, the Rh antibody," Gorman explains.
"The Rh antibody comes back through the placenta, back into the baby and it destroys the baby's red cells."
"These babies are born bloated and with brain damage and very often anaemic, and they very often die. It was a nasty disease," McCluskey says.
First pregnancies are usually safe from Rh disease but, in subsequent pregnancies, the mother's activated antibodies attack the unborn baby.
'The solution was the problem'
John Gorman's brilliant idea came after reading a chapter in Australian Nobel laureate Howard Florey's textbook "General Pathology" in 1958.
Page 703 of Florey's book reads: "The presence of circulating antibody, whether produced actively or received passively, depresses and may completely inhibit the immune response to the relevant antigen."
"Well, I knew in five minutes after I read that, that this would stop the Rh antibody," Gorman says.
"That, if we gave the mothers Rh antibody, they would not make any themselves.
"The solution was the problem: If you re-injected the antibody, you would stop it. It's really ironic that the drug that protects the mothers is exactly the same material that kills the babies."
"John's idea was very paradoxical to many people," McCluskey says.
"The paradox is that the antibody that you're injecting in mothers to mop up [the baby's] Rhesus-positive red cells, is an anti-Rhesus antibody — the very antibody you're seeking to prevent from forming in the mother, and that is a paradox and that scared a lot of people."
How to test the theory?
Well that was the theory, but how to test it, and on whom?
New York's notorious Sing Sing maximum security prison found Gorman and his research partner, Vince Freda, willing male volunteers in the early 1960s.
"It was kind of what was done in those days," Gorman says.
"Today it's an absolute no-no, but in those days, it was kind of [the] custom to ask the prisoners whether they would volunteer to be subjected to experiments and it took Vince Freda a year at the governor's office to get permission."
The Sing Sing trials generated almost perfect results — those exposed to Rh positive blood cells didn't have an immune response if they were injected with passive antibodies.
However, advancing Gorman's theory required a different test subject.
A willing sister-in-law
"They needed a woman, a pregnant woman preferably, to sort of prove that they were right," says Kath Gorman, the wife of John's late younger brother Frank.
As it happened, she was the ideal candidate to trial the treatment.
Kath was expecting her first child in 1964 and is Rh negative. Frank, however, was Rh positive, which put their subsequent babies at clear risk of developing Rh disease, should the baby trigger an antibody response in Kath.
"We had their guarantee that it would give me no after-effects. Again, we did think about that, but we thought, 'Well, in for a penny, in for pound. We'll do it'," she says.
"We wanted more children, so we went for it."
John and Frank's father, a Bendigo GP, had closely followed the Rh trials at Sing Sing and Columbia. Upon learning of Kath's Rh status he had been quick to encourage her to take the antibody.
"She was a nurse and so she realised the clinical situation and she knew about the success at Sing Sing," Gorman says.
"We knew that there had been … zero side effects, so she just made a rational decision."
The ice box
But getting a vial of experimental human antibody to Kath Gorman from New York was no small feat.
She and Frank were living in London at the time and there was no approval on either side of the Atlantic to administer the experimental biological product to a pregnant woman.
John Gorman and Vince Freda went to the TWA freight terminal at New York’s JFK Airport with a box and accompanying paperwork describing the contents as “HUMAN SERUM”.
"This was apparently totally illegal. You weren't allowed to ship an unlicensed drug out of the country," John says.
"They shipped it in a foam container with frozen ice," Kath recalls.
Kath and Frank Gorman headed to London Heathrow to pick up the parcel, thinking its contents wouldn't be needed for another week or so, when the baby was due.
"We were on the way up to the airport to pick it up … and my stomach feels funny. I said to Frank, 'My stomach keeps going hard', and he leant over and he felt and he just said, 'Oh you stupid thing, you're having contractions!'"
After picking up the antibody at Heathrow, they rushed to Barnet Hospital.
The doctor on call was told of the Rh vial in the ice box and informed of the experimental treatment.
After some delay, the doctor telephoned researchers in Liverpool, who had also been studying Rh disease, and despite being research rivals, they told the doctor to administer the antibody.
"I thought this was extremely generous," Gorman says, "because this was probably illegal and meant that we beat them to be giving the first dose, because we were kind of competitors."
Kath remembers the moment well: "The English were a little bit annoyed, because it was an American injection given to an Australian woman in an English hospital."
As for the potential risks involved in taking the injection: "I don't think we thought about it. I think we thought that, 'Yes, we wanted extra children, you know, and that we hoped John's injection did work and that for John's sake, we hope it worked, as well as our [sake]'."
It worked exactly as hoped. Kath didn't develop antibodies from having Rh positive baby Kieron, and a year later in 1965, she had Angus.
"He was 10 pounds, bellowed like a bull and sort of wanted to be fed," Kath says of baby Angus.
"He proved, by being healthy, that John's injection had worked. And, therefore, in medical history, he sort of became, as he calls himself, 'the miracle child'."
John says: "The fact that Angus was safe in Kath's next pregnancy was a wonderful result."
John Gorman's breakthrough treatment, officially called RhoGAM in the US or Anti-D in Australia, was major medical news.
So much so, he even appeared on NBC's Today Show with Barbara Walters in October 1967 to go over the discovery.
"His work, realising that you could eliminate haemolytic disease [breakdown of red blood cells] of the newborn due to Rhesus incompatibility by giving the mothers anti-D immunoglobulin or antibody, I would suggest has saved millions of lives," McCluskey said.
"We need to make people aware of our heroes, the people who've achieved great things on the international stage and changed the world.
"[Gorman] was, without any question, a great pioneer of a new treatment that has all but eliminated a nasty disease."
But what of Gorman's very first patient, Kath Gorman?
After Kieron and Angus, and adopting Ian, she gave birth to four more children.
"Six under seven and then we went four years for Jacob — so we had seven under 11 and that was very good. Then we just stopped, no more came."
Gorman's one regret
John Gorman — now 91 and living north of San Diego — says he was lucky to work with dedicated and determined researchers, including Vince Freda and immunologist William Pollack.
"It's very great satisfaction to see something like this work and now be put in place as part of medical practice and everything's working extremely smoothly. No question, wonderful feeling," he says.
In 1980, Gorman, Freda and Pollack were awarded the Albert Lasker Clinical Medical Research Award for their work on Rh disease.
However, Gorman has one regret and one remaining ambition.
"I'd really like to see the job completed so that, in undeveloped countries, babies don't have to suffer from Rh disease," he says.
Gorman is a member of WIRhE, an international consortium of doctors and scientists working to eradicate Rh disease worldwide.
"I regret the fact that we had the idea ready to go in 1960 and it wasn't approved by the NIH (National Institutes of Heath) until 1968," he says.
"So, for eight years, those babies were dying. Really no reason why it couldn't have been put into action in 1960, because the drug is known to be safe."
In Jim McCluskey's eyes, John Gorman should be a household name.
"John Gorman is someone who should be a lot better known," McCluskey says.
"His contributions are comparable to the achievements of Ian Frazer with the Gardasil vaccine, Fiona Stanley's work in public health and Aboriginal child health, the fundamental science of Peter Doherty and Sir Gustaf Nossal.
"John Gorman's name should trip off the tongue, along with those amazing people who created a scientific Australian scientific legacy."
Credits
Reporter: Andrew Probyn
Production: Georgia Hitch
Videography: Matt Roberts, Luke Thomas, Simon Beardsell and Scott Jewell
Video editing: Jan Pritchard