This story contains discussions of suicide. If you or anyone you know is in need of support, you can contact the national Canadian suicide hotline at 1-833-456-4566.
When preparing to take a call from a person in distress—sometimes a person on the verge of taking their own life—you need to first develop a ritual.
For Emjay Wright, a twenty-five-year-old hotline responder who worked at the Distress Centres of Greater Toronto in 2019 and 2020, that ritual would unfold on the twenty-minute walk from their home near Kensington Market to the office. Walking down lively, prepandemic Queen Street, emotionally and physically preparing for the calls they were about to take, Wright would turn their intentions over in their mind, thinking about their reasons for serving at the hotline.
“Every time I’d hear a siren, every time I’d see an ambulance, they might be going to someone who is suicidal,” says Wright. “The people walking by could be people that I’m talking to that night.”
As they walked, Wright would go over the steps a responder takes when hearing from a suicidal caller: understanding where that desire to end their life is coming from and gently guiding them away from it. The goal was to be able to learn as much about the caller as they could with the fleeting time they had “so I can not just care for them but remind them of what they already do to care for themselves.”
But the night shift was a different beast. Someone calling at 3:00 a.m. simply doesn’t have the same supports available to them. Programs for people with addiction or mental health concerns, food banks, employment support agencies, social services—none operate 24/7. Callers also hesitate to reach out to loved ones, feeling like more of a burden for calling in the middle of the night than during the day. An overnight shift on the hotline feels, overwhelmingly, like just you and the caller, alone. During those calls, Wright says, “I would remind myself that the morning is coming.”
Wright still remembers one such call early in their time as a volunteer. It was around 5:00 a.m., and the caller was in the process of attempting to end their life. The call lasted an hour and a half, with Wright trying to listen and deescalate.
Their shift was coming to an end, but they stayed on the line with the caller to devise a plan for daybreak: people they could talk to, ways to try to ensure they weren’t brought back to the point they’d been at earlier that night. When someone calls intending to end their life, it’s natural for a responder to feel fear. But, more than that, Wright says, they felt the sense that a door had opened—this person had called the hotline. “[I felt] gratitude to whatever part of their body was resisting the urge to end their life.”
Crisis hotlines are, in essence, the emergency rooms of the mental health world. Their responders are a national labour force of largely volunteer frontline workers, driven by a desire to do some good. Distress Centres, one of the largest crisis hotlines in the GTA and an amalgamation of formerly separate services across Toronto and Peel Region, has around 500 volunteers. In any given shift, it supports lonely and hurting callers who just need someone to talk to, or who are searching for resources for mental health support, addiction, housing, food, and other essential needs; some of the time, responders work to bring callers back from the brink of self-harm and suicide.
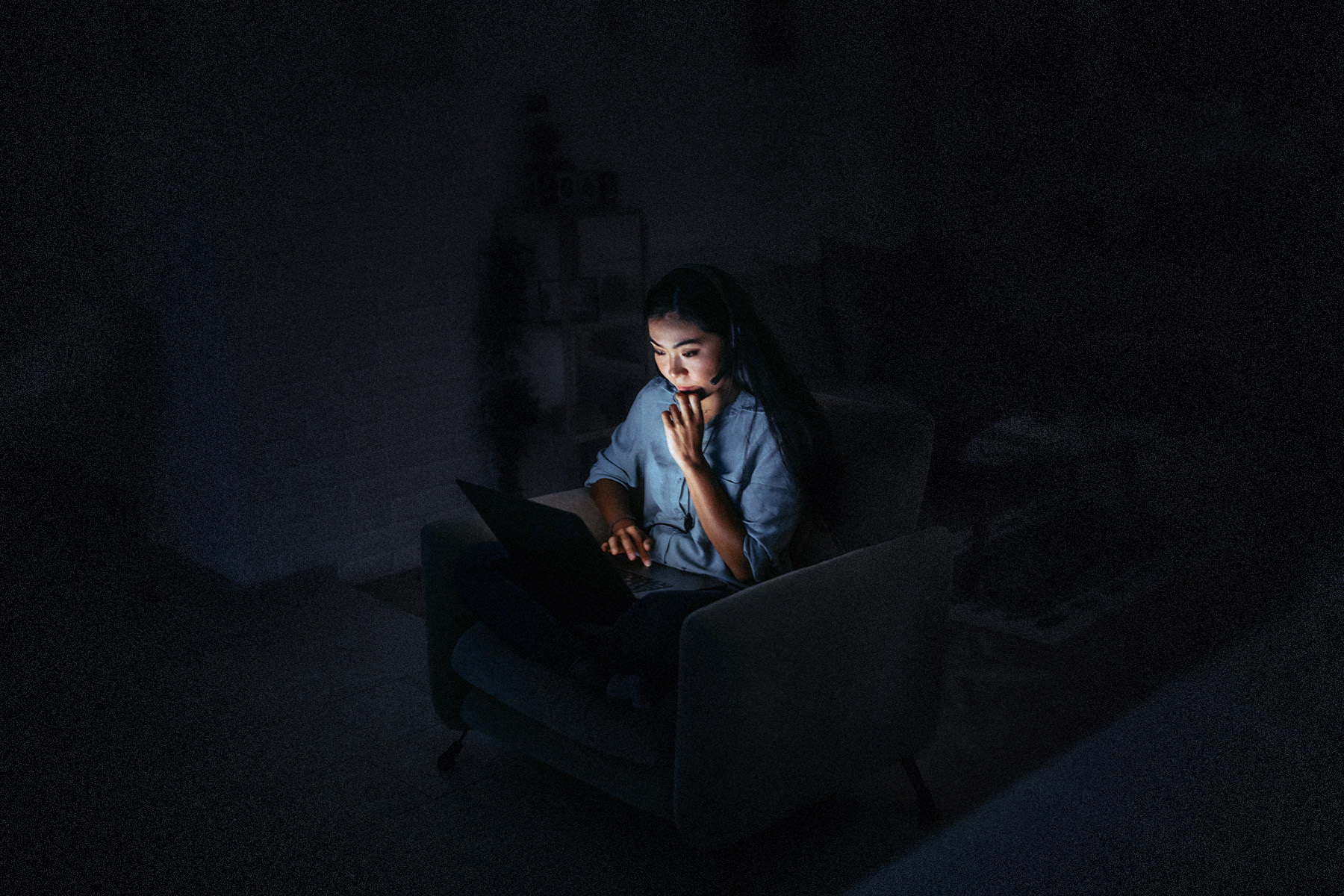
For the sixty or so years that crisis hotlines have been around, the essence of the work has remained remarkably similar. But now, across the country, hotlines are undergoing a period of enormous transition. The shift to a permanent hybrid work setting—with more and more people taking calls from home—happens to overlap with the introduction of the three-digit national suicide number, 9-8-8, next year, changing both the ways that volunteers do their work and likely the scale of the calls they’ll be taking. The isolation that volunteers like Wright experience while on the night shift has intensified as they sit alone in their homes at 3:00 a.m., trying to save lives and comfort the lonely while the rest of the city is asleep.
“The thing about the overnight shift is just the incredible loneliness of it. It’s you in your room by yourself in the middle of the night”
The crisis hotline began with a simple, radically empathetic idea: that a person alone and in pain might not just be comforted but actually saved by a stranger’s voice on the other end of a telephone line.
The US has a rich history of underground hotlines by and for marginalized communities, like abortion provision lines, centres for queer community members, support services for domestic and sexual violence. But the same isn’t quite true in Canada. Many of the country’s oldest, more prominent lines were founded and supported by progressive religious organizers, becoming independent only in later decades.
The first iteration of the Distress Centres was a single Toronto branch founded in 1967 by clergyman Graham Cotter, the head of the Anglican Information Centre, an agency that referred people in distress to resources that might address their needs. A 1969 Saturday Night article describes Cotter as “impressed with the amount of despair and helplessness he found among many of the people his Centre tried to serve.” Seeing the need for a telephone crisis intervention service, Cotter went to England to meet the founder of Samaritans, a British suicide hotline. The Toronto Distress Centre was formed in 1966, run first by a former UK Samaritans branch leader and then by Gordon Winch, a United Church minister known lovingly as the “Padre of the Pubs” for his outreach and support work at bars, where he drank ginger ale and counselled the city’s loneliest and most vulnerable.
In the days before the line opened on November 1, 1967, the organizers distributed yellow calling cards to the city’s bartenders, taxi drivers, pharmacists, and anyone else who might be witness to the loneliness and suffering of the city’s residents. “Give the number to anyone you think might need us,” the organizers said. Their team boasted sixty-one volunteers, covered seven languages—English, French, German, Hungarian, Dutch, Japanese, and Swahili—and had a budget of about $22,000. By 1970, they were receiving 12,000 calls a year.
Since the ’60s, the scale of the service and the societal contexts in which it takes place—particularly when it comes to the stigma and taboos around suicide and mental health and conversations on addiction, poverty, domestic conflicts, and more—have changed radically.
“Don’t forget that the crisis hotline started at a time when making a suicide attempt was still illegal,” says Karen Letofsky, who spent thirty-eight years working at Distress Centres, including as executive director. “People were doing time in the Don Jail—the typical sentence was six months for a failed suicide attempt. So it was, in fact, quite revolutionary to start a distress centre hotline at that time.”
The demographics of the volunteers have also seen a massive shift. “The truth of the matter is helplines originally were built on the backs of housewives,” Letofsky says. “While your typical responder now is leading the same kind of stressful life that callers often are: going to school, working, having family responsibilities. They come to their shift carrying their own stuff.”
That baggage only grew during the pandemic, for both callers and volunteers. Like every other health care service, starting in 2020, crisis hotlines saw a spike in their levels of demand as people faced new kinds of mental health concerns and forms of isolation. Between 2019 and 2021, the number of support interactions across all Distress Centres programming increased by roughly 13,000. Robert Ridge, executive director of Distress Centres, estimates that demand went up by 20 percent at the peak of the pandemic.
The same trends showed up at the national suicide hotline. “We know that there’s increased distress,” says Allison Crawford, Talk Suicide Canada’s chief medical officer. “And many people are hopeful that stigma around mental health, mental well being, mental illness, has decreased. So it makes people more likely to reach out for help.”
At the same time, volunteers were being settled into their home setups—receiving headset deliveries, installing the call software onto their home computers—and taking on an entirely new way of doing work that has otherwise stayed mostly the same for decades. Remote work opens some doors to volunteers who would have been unwilling or unable to commute to an office. But, to some, it also makes an already difficult job even harder, especially on the overnight shift, where responders are suddenly experiencing levels of isolation akin to those of their callers.
The office where the Distress Centres responders once used to work was designed with the intent of being homey and comforting. Letofsky and Wright describe it in nearly identical terms, decades apart: warm, soft lighting, a couch for naps, and a steady supply of snacks. The desks were spaced a few metres apart: you had enough privacy to guarantee the caller only ever heard you, but in your periphery, the hum of voices was a reminder that you weren’t doing this work alone.
Now, with responders largely working from their homes, that sense of community is more elusive. The early hours of the night are some of the worst for crisis calls, no matter where you go in the country. Distress Centres of Greater Toronto is one of the region’s primary hotlines, taking calls from both its own local number and through the national suicide hotline, run by Talk Suicide Canada, an organization supported by the federal government and run by the Centre for Addiction and Mental Health (CAMH). This means that calls can come in from across the country when hotlines local to the caller don’t have the capacity to answer. As midnight moves westward across the country, calls from those regions spike and then drop—a national wave of crisis and sorrow peaking in each time zone between 8:00 p.m. and 12:00 a.m. Only once it’s 4:00 a.m. in Toronto does the line start to quiet for the night.
And the loneliness of the work—which feels more manageable during the day—becomes stark and unbearable at night. You can’t turn to your colleagues after a difficult call. With the need for confidentiality and with roommates and family asleep, it’s difficult to find anyone to lean on at home—and harder still for some to reach out to their shift supervisors without feeling inadequate for not processing the calls independently. And the rituals have changed: in your room, while most of the rest of the city is asleep, distinguishing between your full self and the version of yourself answering the calls has become more challenging.
“When I was serving on the hotline, I was really only being a part of myself . . . I am playing a role, in a way,” Wright says. “To not be able to detach from that role for a moment and have a person-to-person connection that isn’t in aim of providing a service for someone would definitely make it a lot more lonely and make it a lot more inhuman for me.”
Christine volunteered with Distress Centres from 2020 to 2022 and never got the chance to experience what working alongside her fellow volunteers could feel like. (She has been given a pseudonym given her ongoing work in mental health in the city.) Instead, her ritual of preparation for an overnight shift was an intimate routine confined to her Parkdale apartment: waking from a nap around 11:45 p.m., she’d set up a pillow and blanket on the couch in her home office for her midshift break, gather tissues, water, and paper for her copious notes, and go through any notes or feedback from her previous shift. Her window looked out eastward onto the glittering city skyline, whose lights dimmed fractionally as the night went on. Occasionally, she’d hear her partner snoring in the other room, a reminder that she wouldn’t be able to vent to him—or anyone, it seemed—for the next six hours.
“The thing about the overnight shift is just the incredible loneliness of it,” Christine says. “It’s you in your room by yourself in the middle of the night—you have these very difficult conversations with people, and there isn’t a lot of opportunity to debrief.”
“And it’s hard to build relationships with the shift supervisors when you’ve always done the work remotely and have never been into the office.”
Christine could feel a difference in her own well-being at the end of the night based on which supervisor was working—ones who made it clear they were available and responsive or the ones who you know are there but whose presence you don’t feel. She even started scheduling shifts to align with the more responsive supervisor’s.
Ridge, executive director at Distress Centres, is aware of the concern. Before the pandemic, Distress Centres had five facilities in the GTA—by the end of 2022, it had just one, in an innocuous old house in Mississauga. He understands the challenges remote work poses but acknowledges the organization is in the early stages of understanding how to address it.
“When the pandemic first hit and we had to start equipping people to work virtually, the one immediate issue that we were faced with was how people could debrief after a call,” he says. “It’s not a challenge that can’t be overcome, it’s just that it requires new processes and practices to be in place to manage that call.”
With remote work of this nature, the risk of burnout seems to come faster. Christine always knew she wouldn’t be able to do the work forever, but her limit became clear after a particularly difficult overnight call this past summer involving more than seventy minutes of deescalation and an active rescue of the caller by emergency responders. All she got from her supervisor was a quick message saying, essentially: great job, take a break. For Christine, the alienation from the work had set in.
Wright left the hotline some months into the pandemic not only because of the emotional weight of doing the work remotely but also the logistical concerns—they lived in a home with roommates who they tried to be careful not to disturb, and their poor internet connection was a liability during their shifts.
“Whether technological or emotional, I didn’t have the resources to continue doing remote calling,” they say. They’d love to be able to return to doing the work someday—but they know that the most likely way that’ll happen is if the camaraderie of an in-person workspace could somehow be preserved.
The pandemic has transformed a system that has been relatively stable for sixty years, and it’s unclear what effect it will have on the volunteers holding up the practice. It’s not that the shifts won’t happen anymore. We know that volunteers will still show up, reliably, to lend an ear to the people who need it. Strangers will still connect for a fleeting moment each night, bettering some lives, outright saving others. But there’s no telling in what state they’ll meet the morning.







