
It’s Sexually Transmitted Disease (S.T.D.) Awareness Week, so as a special treat the Centers for Disease Control and Prevention (C.D.C.) released the 2020 S.T.D. Surveillance Report, which found that incidences of these infections continued to increase in the midst of the pandemic.
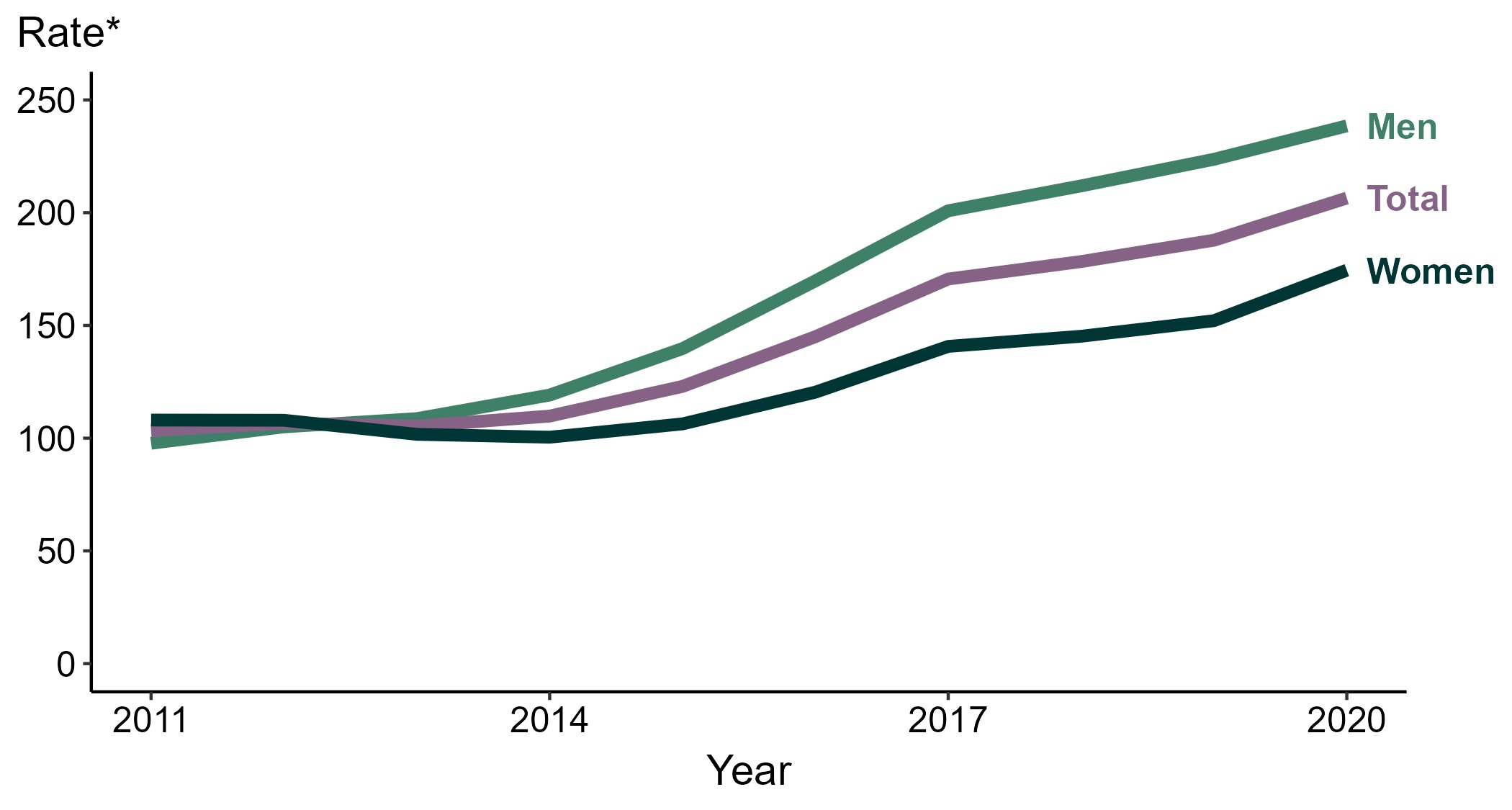
In particular, 677,769 cases of gonorrhea were reported to the C.D.C. in 2020, which is a 45 percent increase from reported cases in 2016.
The good news is gonorrhea is curable, but the disconcerting news is that it’s becoming more antibiotic-resistant. This could eventually lead to an untreatable strain of gonorrhea. In 2016, the World Health Organization set a target to reduce gonorrhea incidences by 90 percent by 2030. A hefty part of that effort is geared toward developing a gonorrhea vaccine.
A vaccine specific to gonorrhea currently doesn’t exist, but three studies published this week in the journal The Lancet Infectious Diseases examined the effects of a vaccine for a different infection and found that it was at least 26 percent effective against gonorrhea. This multitasking vax? MenB-4C which is currently licensed for use against meningitis, a condition that arises from meningococcal disease, an illness caused by the bacteria Neisseria meningitidis.
What’s new — These three research teams aren’t the first to propose using a meningitis vaccine for gonorrhea prevention, but they present new, promising findings.
One study comes from the C.D.C., and looked at the MenB-4C vaccine in more than 40,000 people, aged 16 to 23 years old, living in New York City and Philadelphia with gonorrhea. Using immunization registries, the researchers looked at who had received zero, one, two, or three doses. They found that a complete round of MenB-4C was 40 percent effective against gonorrhea. Even partial vaccination was 26 percent effective.
“A vaccine, even of modest effectiveness and duration of protection might have a substantial effect on gonorrhea prevention,” Winston Abara, an epidemiologist at the C.D.C.’s Division of S.T.D. Prevention and one of the study’s authors, writes to Inverse.
These findings are an improvement from a 2017 study from New Zealand published in The Lancet that found another meningitis vaccine, MeNZB, proved 31 percent effective in protecting against gonorrhea.
Another study from the University of Adelaide in Australia looked at the vaccine’s effectiveness against gonorrhea in adolescents two years after injection. Two doses of MenB-4C was associated with a lower risk of gonorrhea, with a 30 percent effectiveness.
The last study from Imperial College London went a step further and used mathematical modeling to estimate how using the meningitis vaccine to treat gonorrhea could financially impact the National Health Service England’s publicly funded health care system and prevent cases. Specifically, they focused on men who have sex with men, a population that comprises nearly half of the gonorrhea cases in England according to the study’s lead author. By the researchers’ estimates, vaccination could prevent 110,000 gonorrhea cases in England and save £8 million — more than $10.4 million — over 10 years.
“You’re averting all of these treatment episodes,” lead author Lilith Whittles tells Inverse. Whittles is an infectious disease modeler and postdoctoral fellow at I.C.L.
Why it matters — Perhaps it doesn’t need to be stated why it’s a good thing to lower one’s risk of an unpleasant, potentially life-threatening S.T.D., but better to be explicit.
Gonorrhea is caused by the Neisseria gonorrhoeae bacterium, and can affect the genitals, rectum, and throat. Condoms protect against transmitting it. If someone with gonorrhea is pregnant, the baby is at great risk of health problems and developing the infection during birth. Some symptoms of this S.T.D. include:
- Burning sensation while peeing
- Painful or swollen testicles
- Increased discharge or irregular bleeding from the vagina
But gonorrhea doesn’t always present symptoms, which makes it even scarier that there are severe, permanent health risks to going untreated:
- Increased chance of getting or giving H.I.V.
- Formation of scar tissue that blocks fallopian tubes
- Pregnancy outside the womb (ectopic pregnancy)
- Long-term pelvic and abdominal pain
There is a cure — one 500-milligram shot of ceftriaxone — but there are antibacterial-resistant strains of gonorrhea, which could result in an untreatable infection.
Digging into the details — This two-for-one works because the bacteria N. meningitides and N. gonorrhoeae are quite similar. According to the paper from the University of Adelaide, antibodies from MenB-4C recognize proteins in gonococcal bacteria and fight against them.
Whittles from the I.C.L. study also recognizes this overlap between the two bacteria. “They often hang out in the same areas of the body, and they can even swap genes,” she says.
While it’s convenient for now that one vaccine protects against these two infections, Whittles wonders if the middling effectiveness against gonorrhea would deter patients. “If you offer the vaccine to people in sexual health clinics, how many people are going to opt for that, especially because of the issue of imperfect protection?” she tells Inverse. “That might not be a huge motivator for people to take it.”
What’s next — The hope is that eventually there will be a vaccine specifically for gonorrhea with a much higher effectiveness. “This meningitis vaccine is a stopgap,” says Whittles.
Even this stopgap can be of use in developing a gonorrhea-specific vax. “These findings provide further evidence supporting the feasibility of an effective gonococcal vaccine for gonorrhea,” Abara from the C.D.C. writes to Inverse.
For the time being, the meningococcal vaccine regimen fights against more than meningitis; and consider this an evergreen reminder to get tested regularly for S.T.D.s since ones like gonorrhea don’t always present symptoms.







