
Sixteen children have now died from conditions related to the Strep A bacterial infection after outbreaks hit a number of schools and left hospital A&E departments “overflowing” with young patients.
The infection has hit the NHS during its busiest period time, with pharmacies struggling with localised shortages of antibiotics – leaving parents struggling to find medicine for their sick children.
Dr Adrian Boyle, president of the Royal College of Emergency Medicine, said: “There is significant pressure in our paediatric departments, and it’s not just worried parents with Strep, its persistent problems that we’ve got with RSV and flu.
“We think we’re seeing a doubling of paediatric attendances, part of the problem is group A Strep does require some face-to-face consultation.”
Have you been affected by this story? Contact zoe.tidman@independent.co.uk
Health authorities are now investigating the recent increase in Strep A cases while parents have been urged to be vigilant and stay on the look out for potential symptoms.
But what do we know about the outbreak so far?
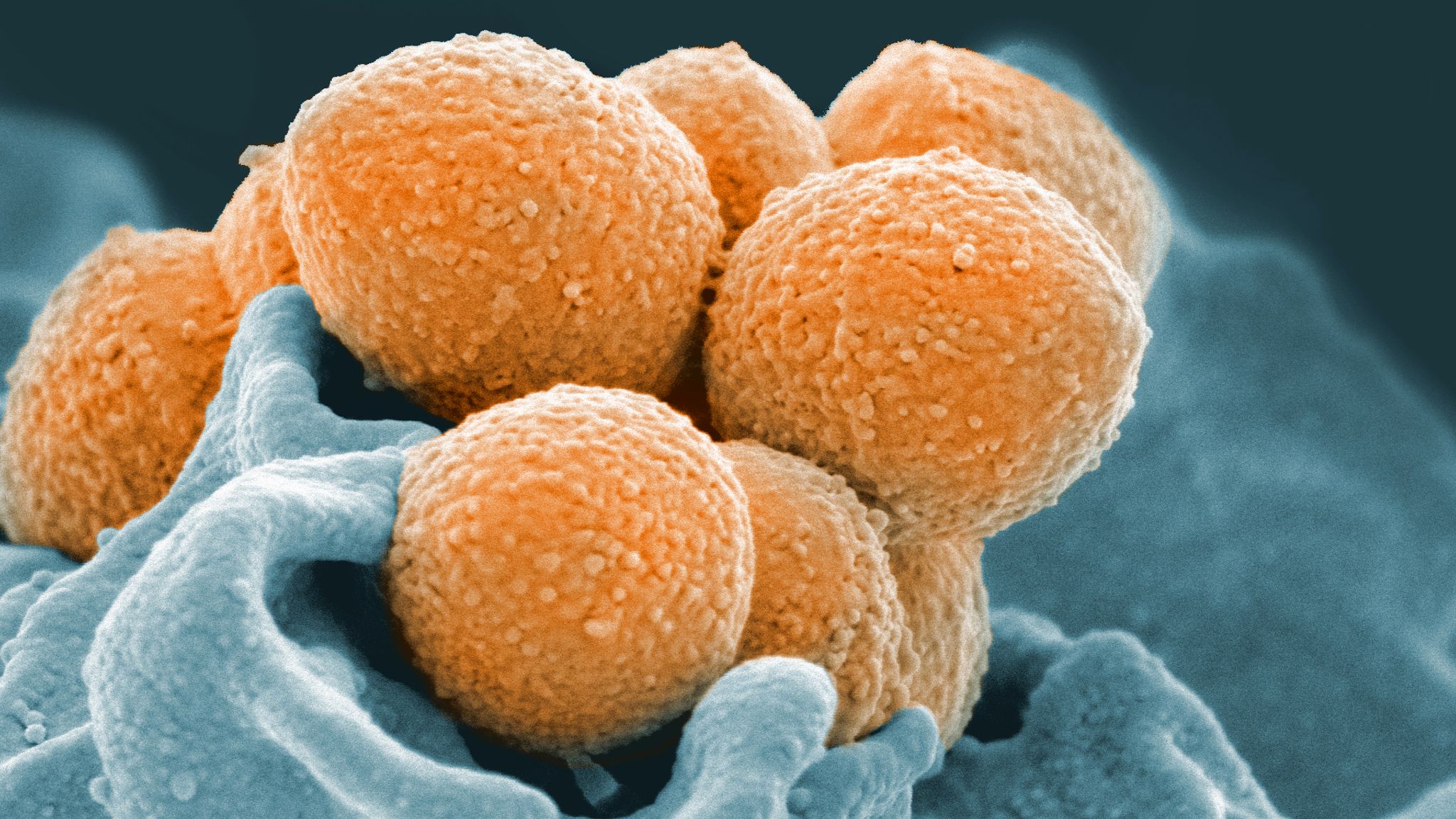
What is Strep A?
The bacteria can cause many different infections, ranging from minor illnesses to deadly diseases. They include the skin infection impetigo and strep throat, as well as scarlet fever.
Strep A can also, in rare cases, cause the life-threatening invasive Group A Streptococcal disease (iGAS).
Most people who come into contact with Strep A bacteria, however, remain well and symptom-free.

When did the recent outbreak start?
Health authorities say there has been an increase in both scarlet fever and iGAS this year.
The increase is most likely related to high amounts of circulating bacteria and social mixing, they say.
There were five recorded deaths among children under 10 within a week of being diagnosed with iGAS in England this season.
During the last high season in 2017/18, the number was just four.
There have been 2.3 cases of iGAS per 100,000 children aged 1 to 4 compared to an average of 0.5 before the Covid pandemic.
For older children aged five to nine, the rate has been 1.1 cases per 100,000 compared to a pre-pandemic average of 0.3.
Who are the victims?
The UK Health Security Agency (UKHSA) has now recorded 13 fatalities linked to the bacterial infection in England, while one child has died in Northern Ireland and another in Wales.
Previous victims include Muhammad Ibrahim Ali, a four-year-old from Buckinghamshire who died in November.
His mother Shabana Kousar said the “sweet and caring” boy had developed a red rash across his back and was initially given antibiotics. She urged other parents to act if they spotted similar symptoms.
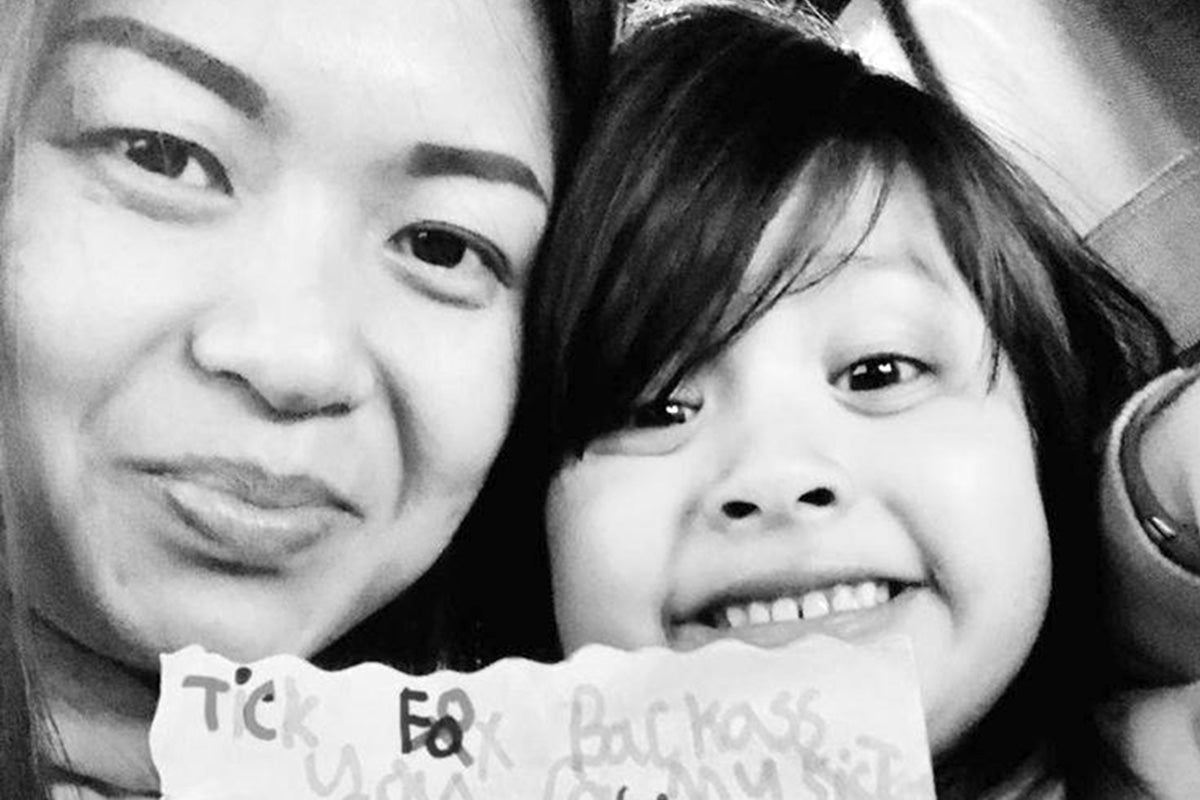
Hanna Roap, a seven-year-old from Penarth in Wales, also died after contracting the infection. Her father Hasan said the little girl was ”always smiling” and the family had been left “numb” after her death.
Other victims have not been identified but include one pupil from St John’s School in Ealing, west London, and another from Ashford Church of England Primary School.
Four year-old Camila Rose Burns from Bolton, Greater Manchester, has also contracted the infection and is currently on a ventilator in hospital.
What are health authorities telling parents?
Dr Colin Brown from UKHSA, said: “We are seeing a higher number of cases of Group A strep this year than usual. The bacteria usually causes a mild infection producing sore throats or scarlet fever that can be easily treated with antibiotics.
“In very rare circumstances, this bacteria can get into the bloodstream and cause serious illness – called invasive Group A strep (iGAS).
“This is still uncommon; however, it is important that parents are on the lookout for symptoms and see a doctor as quickly as possible so that their child can be treated and we can stop the infection becoming serious.
“Make sure you talk to a health professional if your child is showing signs of deteriorating after a bout of scarlet fever, a sore throat, or a respiratory infection.”







