In 2015 Canada's Supreme Court struck down bans on medically assisted suicide as a violation of citizens' liberty, writing that "An individual's response to a grievous and irremediable medical condition is a matter critical to their dignity and autonomy. The prohibition denies people in this situation the right to make decisions concerning their bodily integrity and medical care and thus trenches on their liberty. And by leaving them to endure intolerable suffering, it impinges on their security of the person."
Those quotes, in a nutshell, explain why the ability to end one's life is an important freedom. Our bodies belong to us, not the government. We should have the power to decide whether we wish to continue living, particularly if we are in constant pain or suffering debilitating or fatal illnesses. In the Supreme Court's ruling, the judges note that a ban on physician-assisted suicide "is rationally connected to the goal of protecting the vulnerable from taking their life in times of weakness" but that such protections don't justify a full blanket prohibition on the practice. And so, the court ordered Canada to draft new legislation permitting euthanasia and assisted suicide. The Medical Assistance in Dying (MAID) law was implemented in 2016.
Unfortunately, the philosophical argument for the right to die can also end up colliding with troubling decisions in a country where the government funds and controls access to healthcare. That is reportedly happening in Canada, where some citizens say health officials are actively encouraging people with disabilities and other chronic medical issues to consider suicide.
According to the Associated Press, hospitals are raising the possibility of assisted suicide with patients who hadn't asked about it. These conversations are not motivated by quality of life but health care costs.
The A.P. notes that Belgium and the Australian state of Victoria, which allow physician-assisted suicide, tell medical professionals not to bring up euthanasia so that it's not seen as medical advice. In other words, make sure it's the patient's idea.
This is not the case in Canada, where health care workers are trained to inform patients that they can choose euthanasia if they have a qualifying condition. This has led to some patients, particularly those with disabilities but not necessarily fatal illnesses, having some unpleasant conversations. One provided a recording to the Associated Press:
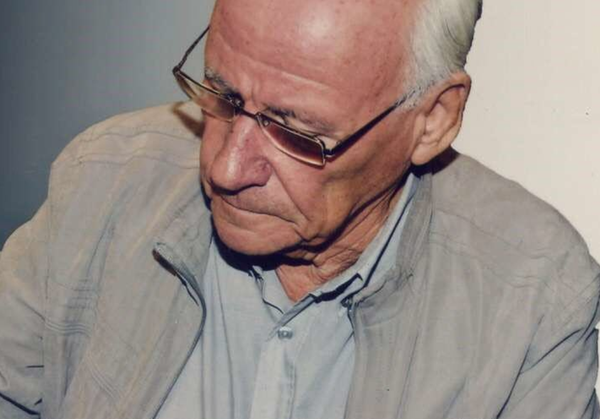
Roger Foley, who has a degenerative brain disorder and is hospitalized in London, Ontario, was so alarmed by staffers mentioning euthanasia that he began secretly recording some of their conversations.
In one recording obtained by the AP, the hospital's director of ethics told Foley that for him to remain in the hospital, it would cost "north of $1,500 a day." Foley replied that mentioning fees felt like coercion and asked what plan there was for his long-term care.
"Roger, this is not my show," the ethicist responded. "My piece of this was to talk to you, (to see) if you had an interest in assisted dying."
Foley said he had never previously mentioned euthanasia. The hospital says there is no prohibition on staff raising the issue.
That Canada's health care system is primarily publicly funded and also has very long wait times for certain types of medical care has naturally raised questions about whether health officials are looking out for patients or what's best for the service providers and government. Over the weekend, this 2017 report on CBC about "potential savings" from assisted suicide was making the rounds on Twitter.
The above-linked report by the Canadian Medical Association Journal was intended to analyze the costs of implementing MAID regulations before the program was rolled out across the country. The report calculated that implementing assisted suicide programs would cost $1.5 million to $14.8 million but could reduce annual healthcare spending by between $34 million to $136.8 million. The report itself wasn't suggesting physicians encourage suicide. It calculated that less than 4 percent of Canadians would use it and that most would likely be dying when they chose to do so and would see their lives shortened by a month or less.
But looking back at that report five years later and looking at the behavior of Canadian health officials now, it's easy to sympathize and agree with concerns that the country is using assisted suicide as a way of trying to "handle" those with chronic, expensive medical issues that require extensive treatment. Tristin Hopper at the National Post notes that there are already several horror stories suggesting people are being pressured to die and that there are questions about whether health officials are making sure patients are of sound mind:
Last June, the Medical Assistance in Dying Committee heard from Trish Nichols, whose suicidal and severely mentally ill brother Alan was given assisted death at a Chilliwack, B.C., hospital in 2019, at a time when MAID was still limited only to Canadians with a terminal illness.
Alan had been taken by his family to the hospital only days before to recover from a psychiatric episode, and in the minutes before he received a lethal injection, Trish described Alan screaming uncontrollably, despite the hospital's assurances that he had opted for a medically assisted death while "of sound mind."
It should be uncontroversial to note that a person voluntarily agreeing to assisted suicide should not be screaming when it happens.
The lesson here should not be that assisted suicide is bad, but heavy government involvement in health care decisions has an inescapable distorting influence. At the very least, how Canada manages health care access is a massive contributing factor. A survey from 2016 found that Canadians wait longer to access health care services than citizens in 11 other countries. The United States is one of the countries of comparison, but the survey also looks at other countries with government-managed health care systems like the United Kingdom and France. A 2020 study from the Canadian Family Physician journal notes that the country simply provides less freedom and opportunity for people seeking medical care than other countries, even when healthcare is centrally planned:
What these countries do differently than Canada is they allow the private sector to provide core health care insurance and services, require patients to share in the cost of treatment, and fund hospitals based on activity (rather than the global budgets that are the norm in Canada).
In absence of significant "freedom" to pursue individualized health care options, Canada is now potentially violating citizens' rights in the exact opposite direction than it was before. People have the right to die but also the right to continue living in the face of medical adversity. That Canada's publicly-operated health care system is unable to efficiently meet the needs of citizens makes all these health worker interactions about euthanasia inherently suspect.
The post Some Canadian Health Care Patients Say They're Being Encouraged To Just Die Already appeared first on Reason.com.