For the last two years, there’s been a mystery boggling the minds of scientists: Why do some people get severe Covid-19 while others get mild symptoms or none at all? The answer, it seems, lies within our genetic codes, particularly those that regulate the immune system.
In a recent study, researchers in the U.K. and U.S. discovered that certain genes associated with systemic lupus erythematosus (SLE) may actually defend against severe Covid-19 infection. While this finding doesn’t necessarily offer any immediate clinical application in treating Covid-19, says Ignacio Sanz, a rheumatologist at Emory University School of Medicine, it may emphasize the importance of more genetic screening or antiviral therapies involving these genes.
“In the world of clinical immunology, we frequently face these counterintuitive situations where a particular immunological defect may contribute to both immune deficiency and also autoimmunity,” Sanz tells Inverse. “This study may offer some additional understanding of how the same type of genetic and immunological defects may result in opposite immune responses.”
The researchers published their work Thursday in the journal PLOS Genetics.
Here’s the background — If you’ve ever heard someone mention lupus, SLE is usually what they’re referring to, though there are other rarer subtypes of the disease. At least five million people worldwide, including 1.5 million Americans, have some form of lupus, with 70 percent of cases associated with SLE; women are more likely than men to be affected, which may have to do with estrogen.
Getting lupus doesn’t exactly boil down to whether you’ve got a gene (or genes), says Sanz, as one’s risk is a complex interplay between DNA, hormones, and the environment. However, the genetics of lupus position it uniquely within Covid-19 since a lot of genes are linked to antiviral responses, the authors explain. (Viruses like cytomegalovirus — related to the same viruses that cause chickenpox — and the Epstein-Barr virus behind mono, also known as the “kissing disease”, are known lupus triggers.)
How they did it — The go-to tool in any geneticist’s toolkit is a genome-wide association study, or GWAS for short. These involve taking a large group of people with a known disease (like lupus) or infection (like Covid-19) and comparing them against a healthy population of folks to see whether the group with lupus and Covid-19 have a distinct set of genes that their healthy counterparts don't have
To find the lupus-Covid-19 association, the researchers took data from three different GWASs searching for genes that made folks susceptible to lupus and compared it against Covid-19 data from the Genetics of Susceptibility and Mortality in Critical Care (or GenNOMICC), which for over the last decade, has looked for genes that make people more susceptible to critical illness or injury than others.
What they found — Comparing the databases, the researchers found several genes associated with an increased risk of developing lupus that seemed to offer a protective and not-so-protective advantage against severe Covid-19 infection. But the one that stuck out the most was TYK2, which encodes an enzyme that regulates interferon production. Interferon is a protein naturally made in response to infections and other diseases like cancer. Specifically, two variants of this gene likely result in higher levels of interferon production, which may sound great when you want to fight a virus but not so much for an autoimmune disease where too much interferon prods the immune system to attack healthy tissues.
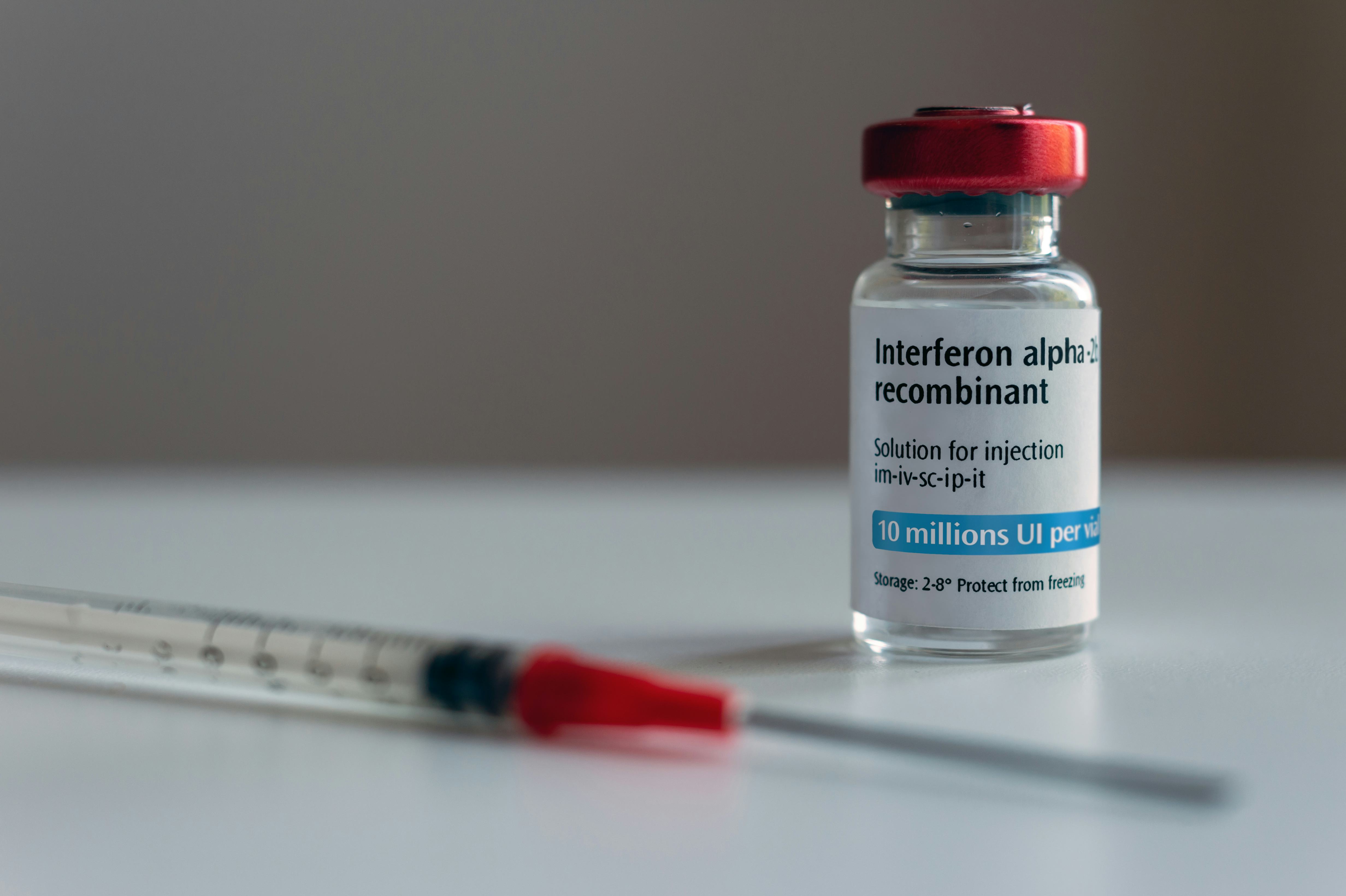
Why it matters — While the study has its limitations — the people studied were mostly of European descent — Sanz says it further illuminates the role of interferon in reducing severe Covid-19 infection.
“[The study] provides another level of genetic understanding of how defects in the interferon response might contribute to severe infection, whether it’s genetic or function because of the presence of antibodies [against interferon],” he says.
So far, clinical trials investigating the efficacy of interferon treatments among hospitalized patients haven’t done well with the exception of one Brazilian trial involving more than 1900 non-hospitalized, high-risk Covid-19 patients, reported Science in May. Eiger BioPharmacueticals, who sponsored the Brazilian trial, was seeking emergency use authorization from the U.S. Food and Drug Administration, which has yet to be approved.
Just to be clear, if you have lupus and are lucky enough to have the “good” version of TYK2 (not exactly knowledge lupus patients are privy to since genotyping at diagnosis isn’t common, says Sanz), that doesn’t mean you’re protected against the virus. Because of the medley of genetic variants involved, there are patients with lupus who don’t necessarily make a crazy amount of interferon, so if they come down with Covid-19, they’re not likely to fare any better than folks without lupus.
“In general, maybe because of the immunosuppression [from the drugs to treat the disease], lupus patients may do worse,” says Sanz.
It’s also important to bear in mind, this finding is only an association — there seems to be a relationship between TYK2 and Covid-19, but it’s not one-and-done. Further studies will need to be conducted with a broader and more diverse population of people and potentially large-scale clinical trials, says Sanz.
In any case, the more information we have to fight this insidious virus, the better.

.png?w=600)