
Tory MP Craig Mackinlay recently returned to Commons for the first time after suffering from a life-threatening bout of sepsis last year. Since his return to public duties, Mackinlay has spoken candidly about his experience with the near-fatal illness that led to the amputation of his hands and feet.
Last September, Mackinlay said he’d begun feeling unwell – but didn’t think anything of his symptoms, especially after testing negative for COVID.
But his condition quickly worsened throughout the night. When Mackinlay was finally admitted to hospital the following day, his entire body had turned blue. He was experiencing septic shock – a severe form of sepsis. Mackinlay was put into an induced coma, waking up 16 days later. He’d had just a 5% chance of survival.
With nearly 50 million cases and 11 million deaths globally each year, sepsis represents a significant global health crisis. Yet despite its prevalence, sepsis remains a perplexing condition to diagnose promptly.
Sepsis is a severe condition that arises when the body’s response to an infection injures its own tissues and organs. It can develop in a very short timeframe – usually hours, if untreated.
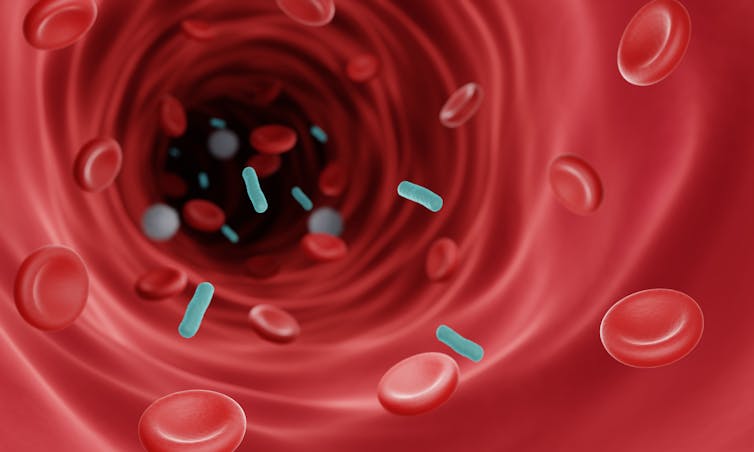
Sepsis is typically triggered by a bacterial or viral infection – often in the lungs, urinary tract, abdomen or from a wound. If these pathogens escape the infected area, they can then enter the bloodstream where they’re able to spread throughout the body into surrounding tissues and major organs.
Because of how quickly the infection spreads, the immune system gets overwhelmed and becomes dysregulated – meaning it stops functioning as it normally should. This triggers an exaggerated immune response known as a cytokine storm. This cytokine storm not only fails to clear the infection, it also causes extensive tissue and organ damage – which may cause severe complications and even death without prompt treatment.
Sepsis can affect anyone – though older adults, infants, young children and people with chronic health conditions (such as diabetes, arthritis, asthma and cancer) are at greater risk due to differences in the way their immune systems function.
Severe condition
There are numerous reasons why sepsis is such a dangerous condition. This largely comes down to how difficult it is to diagnose.
Early sepsis symptoms tend to share similarities with many other illnesses. Often, patients start out with flu-like symptoms – such as fever, rapid breathing and increased heart rate. These can easily be mistaken for other conditions or overlooked entirely.
Yet these subtle signs can turn severe within hours because of how rapidly sepsis progresses. It’s critical that patients are treated as promptly as possible, as for every one-hour delay in treatment there’s an 8% increased risk of death.
Sepsis can also be triggered by a diverse array of pathogens – including bacteria, viruses, fungi and parasites. This makes it challenging to pinpoint the exact cause of sepsis. Since each pathogen requires a different type of treatment, this means lab tests must first be carried out before patients can be given treatment.
And, because of sepsis’s complex nature, it lacks a biological signature (or biomarker) that can reliably be used to diagnose the condition. Biomarkers play a crucial role in diagnosing various illnesses as they indicate the presence and severity of a disease. This means that doctors need to look for other signs and symptoms, alongside laboratory tests, to diagnose sepsis. But these signs don’t always clearly indicate the presence of the condition – at least initially.
Future of treatment
Sepsis is treated with antibiotics or antivirals, depending on the root cause of a patient’s infection. Patients may also need to be given fluids to maintain their blood pressure and oxygen to support organ function depending on their condition. In severe cases, abscesses may need to be drained, infected tissues may need to be removed and a patient may require a ventilator or dialysis to support their breathing and organ function.
Up to 70% of people who develop sepsis survive the condition when it’s treated promptly. When left untreated, the survival rate drops to about 20%.
Around half of people who survive sepsis develop “post-sepsis syndrome” – long-term physical and emotional symptoms that may last for years. Some of these symptoms can include getting ill more often, feeling weak or tired and experiencing mental health problems.
Yet there are concerns that current sepsis treatments are becoming less effective. The overwhelming majority of sepsis cases stem from bacterial infections. This makes antibiotics the primary treatment avenue for sepsis.
But bacteria can evolve to survive exposure to antibiotics, becoming resistant to the drugs commonly used to treat infections. This makes antibiotic resistance a significant contributing factor for sepsis. This resistance can render antibiotics ineffective in eradicating the initial bacterial infection, allowing it to persist and worsen.
But recent innovations in the field may offer hope. Research has uncovered how pathogens adhere to blood vessel linings – a mechanism that allows pathogens to spread throughout the body. Thanks to this discovery, trials have now begun to test whether a drug which targets the blood vessels (instead of the infection-causing pathogens) can stop sepsis and reduce reliance of antibiotics.
Drugs which block pathogens from binding to blood vessels could also potentially even be administered before sepsis takes hold. If this proves effective, it could save millions of lives.
There are also efforts to introduce standardised sepsis protocols in order to improve early recognition of the condition in hospitals and clinics.
Sepsis can happen to anyone. The best way to avoid it is to look after your health. Keeping up to date with vaccinations, practising good hygiene and properly caring for any wounds you get are all important. But if any of the known symptoms of sepsis occur – including fever, chills and low blood pressure – then it’s vital to seek medical help immediately.
Steve Kerrigan has received research funding from Science Foundation Ireland, Health Research Board of Ireland, Irish Research Council and Enterprise Ireland .
This article was originally published on The Conversation. Read the original article.







