The heart is a near-universal symbol of love and one of the most vital organs in the body. Now, to better understand the inner workings of the heart, scientists have recreated the organ's biology in a device the size of a credit card.
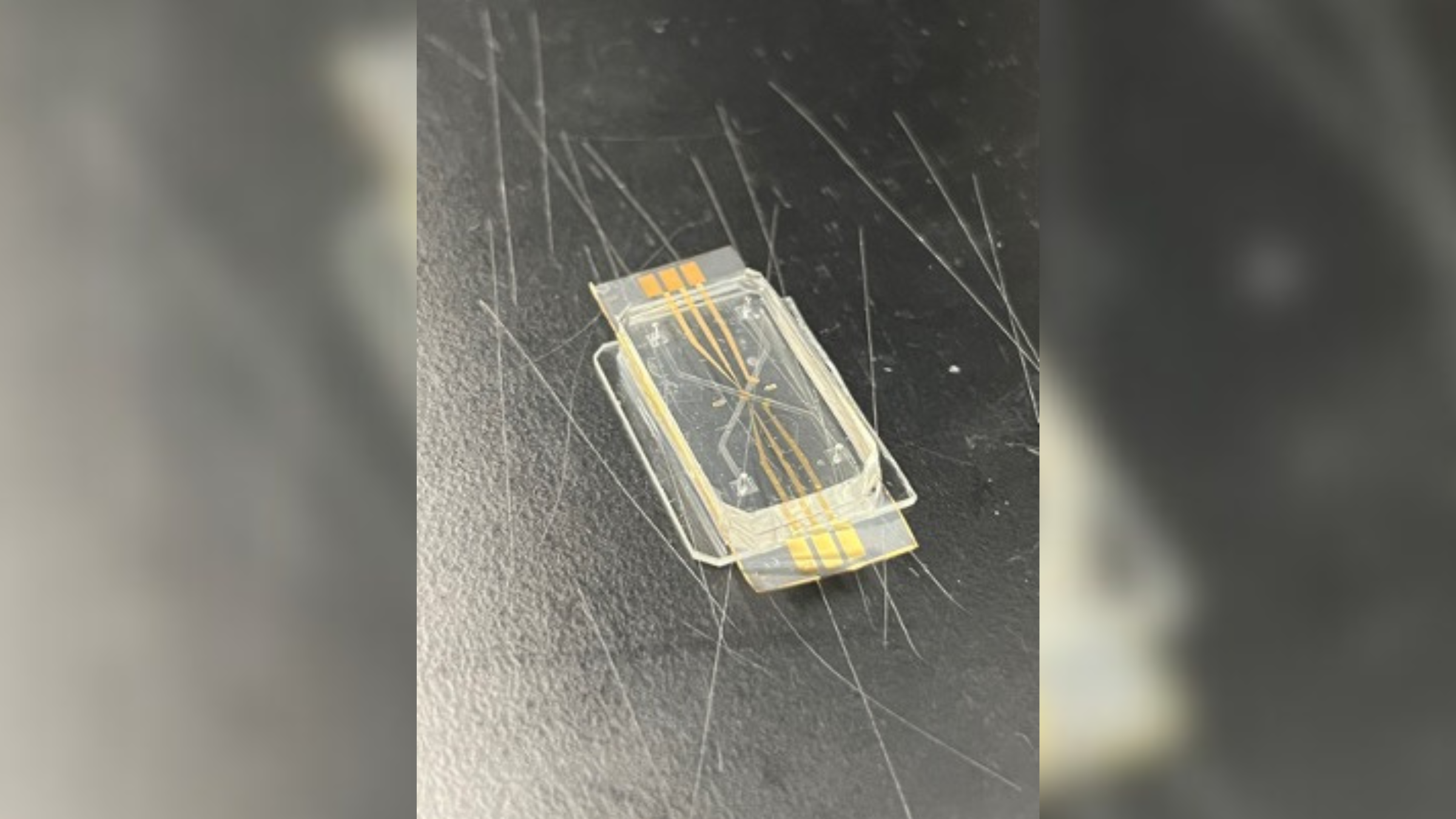
The new "heart-on-a-chip" device, developed by a team from the National Institute of Standards and Technology (NIST), mimics the interactions of cells within a human heart. The researchers say the technology could be used to study heart disease, which is the leading cause of death in the U.S.
Traditional animal experiments — which typically use lab rats and monkeys, among other animals — don't perfectly capture how a disease will progress or a drug will behave in the human body. Because of this, researchers are working to develop more accurate ways of mimicking the complexity and intricacy of human organs in the lab. This accuracy is especially important for drug development, as 90% of candidate drugs currently fail clinical trials in people.
New, human-like models that are being developed include organoids, or miniature organs grown from stem cells, and organ-on-a-chip models, in which cells found in specific tissues are grown on a chip that mimics the physiological conditions of an organ in the body. Many organs have been modeled in such chips, including the lungs, kidneys and the vagina.
Scientists have developed heart-on-a-chip models, in particular, to study how the heart heals after injury, and heart disease, as well as to aid drug discovery. Hearts-on-a-chip have even been sent to space to study the effect of microgravity on the heart.
Related: Tiny 'hearts' self-assemble in lab dishes and even beat like the real thing
In a statement released on Feb. 6, the team at NIST said this kind of technology, which includes their new heart-on-a-chip model, could streamline drug development, making it faster, safer and more precise. Importantly, these models would not replace human clinical trials — they would hopefully reduce or replace the animal testing needed before human trials begin.
"This system could be considered for biomanufacturing and regenerative medicine of the heart and other organs on chips," Darwin Reyes, a biomedical engineer at NIST who led the development of the new chip, told Live Science in an email.
These chips typically have transparent or semi-transparent covers, and by peering inside, researchers can see fluids running through tiny channels that interconnect like streams of water. In the case of NIST's chip, these channels imitate the blood vessels in the heart. Scientists grow human heart cells inside these channels and can study how the cells react to the addition of different drugs into the system.
Unlike existing heart-on-a-chip models, the cells in the new NIST model can be arranged on opposite sides of a porous membrane, meaning that they can communicate with each other via signaling molecules, Reyes said. The next step for the team is to assess how these heart cells behave under normal and stress-induced conditions, he said.
Different organ chips can also be linked together — for example, a liver chip can be linked to a heart chip, which could enable scientists to study how these two organs interact after exposure to a certain drug.
In a recent review of these technologies, published Feb. 6 in the journal Lab on a Chip, Reyes and a colleague emphasized that "significant work" is needed before organ-on-a-chip models can be used in preclinical drug tests. For instance, the heart cells used in these devices are grown from stem cells and often don't fully mature. So instead of resembling adult cells, they resemble cells found in a developing fetus.
Certain materials used in heart-on-a-chip models also need to be refined. Polydimethylsiloxane, for instance, is a polymer commonly used to make the chip, but it's "relatively expensive" and readily absorbs small molecules. That easy absorption can skew scientists' drug tests, making them think that a substance brings about a certain effect or lacks signs of toxicity, when that isn't the case, the authors wrote.
Nevertheless, with further honing, organ-on-a-chip models may cause a "paradigm shift" in the way that new drugs are developed and tested, the team said. The potential of these devices was recognized by the Food and Drug Administration last year, when the agency ruled that they could stand in place of traditional animal testing, as long as the data they generate is robust enough.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!







