
In 2021, a man in his 50s was transferred to the intensive care unit at Emory University Hospital in Atlanta. He was in septic shock due to a bacterial infection that had spread to his bloodstream. The culprit? Klebsiella pneumoniae, which was resistant to most antibiotics.
Finally, hope emerged: A two-week course of an antibiotic called cefiderocol seemed to clear the infection. But just 10 days later, the man was rushed back to the ICU, where doctors discovered a pus-filled mass covering his liver. The same bacteria had returned with a vengeance.
The doctors sent the patient's blood sample to David Weiss, a microbiologist at Emory Antibiotic Resistance Center. Weiss discovered that the bacteria were now highly resistant to cefiderocol.
He quickly notified the doctors. But even after switching antibiotics, the man died.
The man's case highlights an elusive strategy that bacteria use in their arms race against antibiotics — a hidden type of resistance that can be switched on almost instantly but leaves no genetic trace. And it can be almost impossible to detect using standard lab tests. Researchers are increasingly recognizing that this bacterial strategy, called "heteroresistance," may play a significant role in antibiotic failures. Recognizing this bacterial strategy, experts say, is the first step in fighting it.
"While this is a worrisome phenomenon that we're studying now, in the big picture and in the future, I think we'll be able to use this knowledge to greatly help patients," Weiss told Live Science.
RELATED: Superbugs are on the rise. How can we prevent antibiotics from becoming obsolete?
A new kind of resistance
For decades, microbiologists like Weiss thought of antibiotic resistance as something a bacterial species either had or didn't have. But "now, we are realizing that that's not always the case," he said.
Normally, genes determine how bacteria resist certain antibiotics. For example, bacteria could gain a gene mutation that enables them to chemically disable antibiotics. In other cases, genes may code for proteins that prevent the drugs from crossing bacterial cell walls. But that is not the case for heteroresistant bacteria; they defeat drugs designed to kill them without bona fide resistance genes. When they're not exposed to an antibiotic, these bacteria look like any other bacteria.
When typical antibiotic-resistant bacteria propagate, they pass resistance genes to the next generation, creating a legion of antibiotic-resistant populations that collectively counter the treatment. In contrast, bacteria in a heteroresistant population are sensitive to antibiotics. But at certain doses of an antibiotic, a small proportion of this population — as few as 1 in a million — may turn resistant and survive the drugs while the rest of the population stops growing and dies.
Because these resistant cells are interspersed with antibiotic-susceptible cells, it is difficult for microbiologists to detect the resistant ones.
Scientists across the globe have spent years investigating why and how heteroresistance develops so they can get better at detecting these bacteria. Now, new clues are finally beginning to emerge.
Face-to-face with rogue bacteria
Karin Hjort's first encounter with heteroresistance happened by chance. About 10 years ago, Hjort, a microbiologist at Uppsala University in Sweden, was growing bacteria. Strain by strain, she administered lethal doses of antibiotics, labeling any survivors as "resistant" and freezing them. When she thawed out the survivors, she searched for genetic changes, or mutations, that typically underlie their ability to cheat death.
But this time, when she took out the seemingly resistant strains, she "sequenced them and sequenced them" and "didn't find any mutations," Hjort Live Science.
Hjort couldn't figure out what was happening. It seemed as if these bacteria had lost their resistance upon freezing. But then she discovered a decades-old research paper describing a phenomenon scientists at the University of California, Davis called "heteroresistance," in which a population of antibiotic-resistant bacteria could emerge at an unusually fast rate from a seemingly susceptible population.
RELATED: How fast can antibiotic resistance evolve?
In fact, "heteroresistance" was first mentioned back in the 1940s. But the phenomenon is very challenging to study, and without a clear definition, scientists struggle to compare their observations.
"Everyone called out 'heteroresistant' in different ways — there was no standard to look at," Omar El-Halfawy, a microbiologist at the University of Regina in Canada, told Live Science. Some people use the term to describe a situation in which multiple types of bacteria with different antibiotic tolerance levels coinfect a person. Others use it to describe a scenario where two different antibiotic susceptibility tests give different results.
Determined to settle the issue, in 2015 El-Halfawy reviewed every study he could find that described heteroresistance. Ultimately, he decided, heteroresistance occurs when some fraction of a bacterial culture population can withstand a much higher antibiotic concentration than the rest of the population. Scientists adopted this definition in 2015, and the number of peer-reviewed publications on heteroresistance has since doubled.
Fooling the test
The fraction of resistant bacteria in a heteroresistant population can be anywhere from 1 in 1 million to 1 in 10,000. It is so rare that standard clinical microbiology tests easily miss it.
"Essentially, what you're trying to do is detect a resistant needle in a susceptible haystack of cells," Weiss said.
While bacteria often transition from being antibiotic-susceptible to antibiotic-resistant, this transition usually happens in small increments and over at least several days. With heteroresistance, the transition is almost immediate.
The switch between susceptible to resistant and then back again confuses test analyses.
"Every time you grow a strain, it's going to grow a little bit differently," Weiss said. "On one day, it might come up as resistant; on the next day, it might be susceptible. In fact, "having inconsistent, discrepant testing results was like a hallmark of the strain being heteroresistant."
The standard antibiotic susceptibility test goes like this: A population of bacteria, at a fixed density of about 10,000 to 100,000 cells in a milliliter of broth, is dosed with different concentrations of an antibiotic until they stop multiplying or die.
But, according to Hjort, this process isn't designed to spot heteroresistance. Because these standard tests only detect population-wide behavior, extremely rare phenomena like heteroresistance will be missed. "The error is huge, even if we use more bacteria," she said.
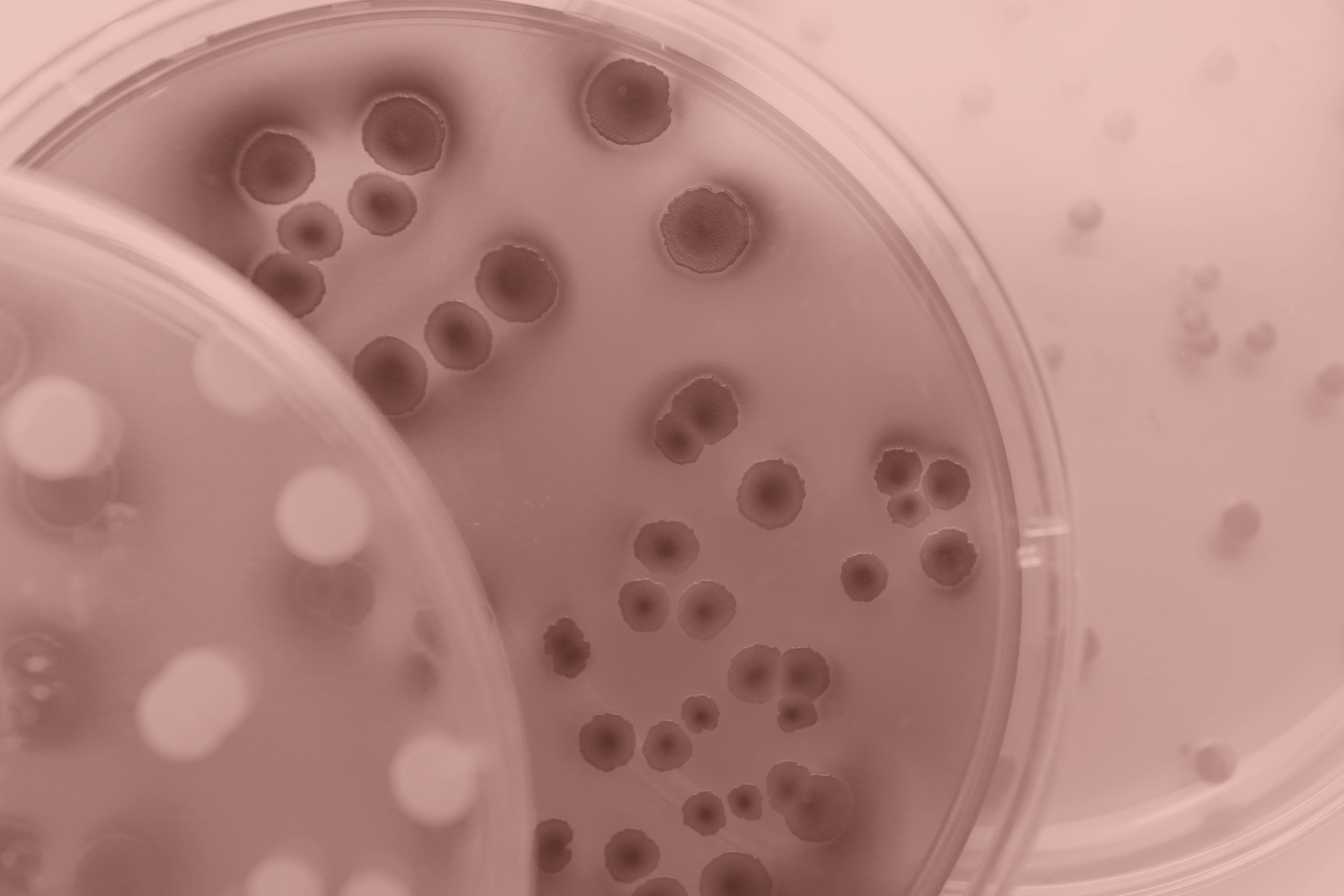
So far, the only method for spotting heteroresistance is called population analysis profiling (PAP). To perform this test, microbiologists grow bacteria overnight, place some on a series of petri dishes containing different concentrations of antibiotics, and monitor the bacteria's growth. Because PAP covers a range of bacterial densities, the test can pick up patterns not normally detected by standard tests.
But the method is laborious, Hjort said. When extra variables — such as the type of antibiotic or the cell densities — are added to the equation, the number of dishes triples or quadruples, said Sofia Jonsson, a graduate student at Uppsala University who works with Hjort.
"If you do a big experiment, it can be 200 plates to count," and each plate may have hundreds of bacterial colonies to count, Jonsson told Live Science. Because it is so tedious, PAP is not routinely done in a clinical setting.
Weiss speculated that to detect heteroresistance, future tests would need to monitor bacteria at a single-cell level and have a 1-in-1-million cell resolution. Some research is already making strides in that direction, he said, but none of these developments have reached the clinic yet.
That's crucial, because with a rapid test, patients with heteroresistant bacterial infections could be given the right medicines from the start, rather than having their illness worsen for days or weeks before doctors try drugs that work.

Cracking the case
Because heteroresistance occurs without permanent genetic mutations, Hjort's team wanted to know whether there were temporary changes to the bacterial genome that could explain the phenomenon.
From Hjort's observation, two groups of bacteria could have at least an eightfold difference in antibiotic tolerance within a heteroresistant population. To figure out why, she tested a handful of multidrug-resistant strains of bacteria such as Escherichia coli, Salmonella enterica, K. pneumoniae and Acinetobacter baumannii against 28 antibiotics. These "gram-negative" bacteria have an outer membrane that shields them from toxic substances. Not a single new class of antibiotic that targets gram-negative bacteria has been approved in the past 50 years.
Using a whole-genome sequencing technique, Hjort and colleagues found that some bacteria became heteroresistant because they temporarily made copies of existing genes that helped them evade antibiotics.
Earlier this year, they expanded the study to include the gram-positive bacterium Staphylococcus aureus that causes common skin infections. These bacteria have no outer membranes, and their resistance mechanisms are generally different from those of gram-negative strains.
Hjort and her team tested for antibiotic resistance against 40 patient samples containing S. aureus that were isolated from hospital patients in Denmark, Norway, Spain and Sweden. Standard tests suggested all of the bacteria could be treated with all six antibiotics.
However, the PAP result revealed heteroresistance to more than half of these antibiotics. These bacteria lacked typical antibiotic resistance genes and hadn't made spontaneous copies of genes that were protective as the gram-negative bacteria had.
Instead, heteroresistance correlated with chromosomal point mutations — changes in single base pairs on various genes — that could be reversed if another mutation occurred. It's still unclear what these mutations do and why heteroresistance seemed to emerge only against certain drugs.
But the variability in how heteroresistance emerges, depending on the drug and species involved, suggests treatment approaches will need to be different, Hjort said.
The quest continues
Scientists have now reported bacterial heteroresistance against almost every class of antibiotics. Hjort thinks a much larger clinical dataset is needed to fully understand the link between heteroresistance and patient outcomes.
A good way to start, she said, is with a proper understanding of how these bacteria develop their heteroresistance in the first place.
Weiss agreed.
By knowing the mechanism of action, "we may be able to develop new drugs that can reverse the heteroresistance and make the bacteria susceptible to the original drug," he said."It's always better to know your enemy."







