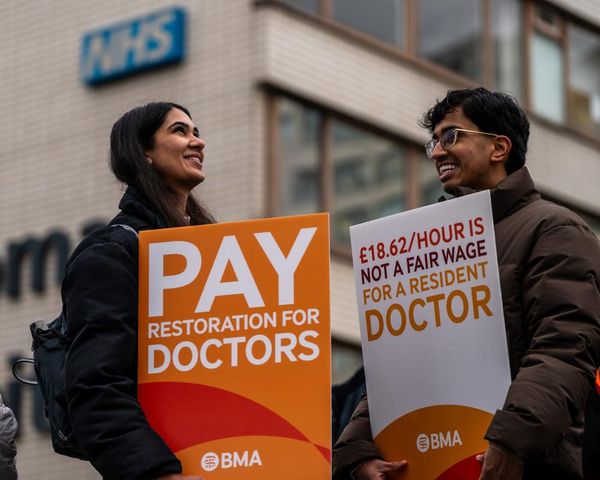
Women in the UK are suffering injuries and other health problems as a result of the growing popularity of anal sex among straight couples, two NHS surgeons have warned.
The consequences include incontinence and sexually transmitted infections (STIs) as well as pain and bleeding because they have experienced bodily trauma while engaging in the practice, the doctors write in an article in the British Medical Journal.
Tabitha Gana and Lesley Hunt also argued that doctors’ reluctance to discuss the risks associated with anal sex was leading to women being harmed by the practice and letting down a generation of women who are not aware of the potential problems.
In the journal, they said “anal intercourse is considered a risky sexual behaviour because of its association with alcohol, drug use and multiple sex partners”.
However, “within popular culture it has moved from the world of pornography to mainstream media” and TV shows including Sex and the City and Fleabag may have contributed to the trend by making it seem “racy and daring”.
However, women who engage in anal sex are at greater risk from it than men. “Increased rates of faecal incontinence and anal sphincter injury have been reported in women who have anal intercourse,” the report said.
“Women are at a higher risk of incontinence than men because of their different anatomy and the effects of hormones, pregnancy and childbirth on the pelvic floor.
“Women have less robust anal sphincters and lower anal canal pressures than men, and damage caused by anal penetration is therefore more consequential.
“The pain and bleeding women report after anal sex is indicative of trauma, and risks may be increased if anal sex is coerced,” they said.
National Survey of Sexual Attitudes research undertaken in Britain has found that the proportion of 16- to 24-year-olds engaging in heterosexual anal intercourse has risen from 12.5% to 28.5% over recent decades. Similarly, in the US 30% to 45% of both sexes have experienced it.
“It is no longer considered an extreme behaviour but increasingly portrayed as a prized and pleasurable experience,” wrote Hunt, a surgeon in Sheffield, and Gana, a trainee colorectal surgeon in Yorkshire.
Many doctors, though, especially GPs and hospital doctors, are reluctant to talk to women about the risks involved, partly because they do not want to seem judgmental or homophobic, they add.
“However, with such a high proportion of young women now having anal sex, failure to discuss it when they present with anorectal symptoms exposes women to missed diagnoses, futile treatments and further harm arising from a lack of medical advice,” the surgeons said.
NHS patient information about the risks of anal sex is incomplete because it only cites STIs, and makes “no mention of anal trauma, incontinence or the psychological aftermath of the coercion young women report in relation to this activity”.
Health professionals’ disinclination to discuss the practice openly with patients “may be failing a generation of young women, who are unaware of the risks”.
Claudia Estcourt, a professor of sexual health and HIV and member of the British Association for Sexual Health and HIV (BASHH), backed the surgeons’ call for doctors to talk openly about anal sex.
“BASHH strongly supports the call for careful, non-judgmental inquiry about anal sex in the context of women with anal symptoms,” she said.
“Within sexual health services, women are routinely asked about the types of sex they have so that comprehensive assessment of likely cause of symptoms, investigations needed and management can be made.
“We find that by explaining why we are asking these questions, asking them in sensitive, non-judgmental ways and giving patients time to answer, are all key to providing the best care.
“We are highly skilled in assessment of women with possible sexually caused anal trauma, whether through consensual or non-consensual sex, and would encourage women with concerns to contact their local sexual health clinic or sexual assault service as appropriate.”