
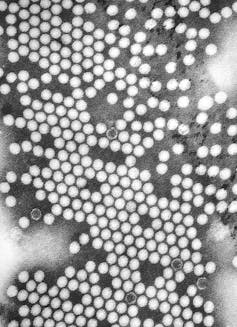
We recently learned that poliovirus had been detected in sewage in north and east London between February and May 2022. Poliomyelitis (polio) is an infectious disease that can cause paralysis and death, mainly in children.
But polio is also a triumph of vaccination. The last known case of polio in the UK was in 1984, and the country was declared polio free in 2003.
While the UK Health Security Agency has said that the risk to the public is very low, the detection of the virus in London’s wastewater has naturally led to a strong public health response. Experts are investigating the possibility of community transmission, and have urged the public to ensure their vaccinations are up to date.
Read more: Poliovirus in London sewage – what you need to know
Polio was detected in sewage as early as 1939 in the US, and today, wastewater is regularly tested for the virus in many parts of the world. Wastewater surveillance for polio was trialled in Scandinavia starting in the late 1960s, paving the way for the World Health Organization to recommend it as part of routine polio surveillance in 2003.
In 2013, a silent outbreak was identified in Israel in this way. Early detection meant that supplementary vaccination campaigns ended the outbreak swiftly in 2014 with no cases of paralysis.
Without wastewater monitoring, the first indication that polio is circulating in a population could be the paralysis or death of a child.

But polio isn’t the only disease we can look for in our wastewater. Wastewater epidemiology involves testing sewage for biological markers of disease that people shed during normal daily activities, such as going to the toilet. These markers could be fragments of genetic materials of a virus or bacteria, for example.
Other pathogens that can be detected in sewage include typhoid and respiratory syncytial virus (RSV), though monitoring for signs of these infections doesn’t happen routinely.
During the pandemic, many countries have employed wastewater epidemiology to track SARS-CoV-2, the virus that causes COVID-19, and to locate emerging variants.
Wastewater surveillance is particularly useful for pathogens where the proportion of asymptomatic infections is high and in countries where clinical surveillance such as testing may be poor. It has been effectively used in low- and middle-income countries to detect diseases like typhoid.
It’s also possible to test sewage for the broken down products of drugs. In this way, wastewater surveillance has been used to track illicit drug use, prescription medication like antidepressants, and even antimicrobial resistance.
The uses for wastewater-based epidemiology can be grouped into two categories. The first is where just the presence of a pathogen requires a response. This is the case for pathogens that have low rates, like emerging variants of SARS-CoV-2 or diseases nearing elimination like polio or measles.
The second is to quantify the burden of a specific disease. In England, 45 sites were sampled frequently for SARS-CoV-2. Our own work on wastewater surveillance for COVID showed it can be used to estimate how common the disease is – that is, the concentration of viral fragments in the sewage reflected the number of cases in the community.
There are some challenges in interpreting concentrations because they can be affected by environmental factors such as the volume of rainfall diluting the samples. But when we know about these effects, we can account for them.
Wastewater epidemiology captures the contributions of almost all the people within a sewage catchment, which can be a double-edged sword. On the one hand, biases that often affect traditional surveillance, such as localised testing shortages or variability in access to healthcare, are reduced. On the other hand, samples collected from large sewage works serve such a large population (over 4 million people in the case of Beckton where the poliovirus was detected) that pinpointing the origins of infection is difficult. Collection of sewage samples closer to the source can help, but is more difficult, harder to analyse and more expensive.
Read more: Testing sewage has helped track COVID – soon it could reveal much more about the UK's health
Budgetary pressure
Overall, wastewater epidemiology can provide unobtrusive, ongoing surveillance for diseases that is relatively cheap and convenient. Sewage testing complements clinical surveillance, especially when infections spread silently or when early detection gives public health officials a useful early warning. It’s a good thing that poliovirus has been identified in sewage before any children showed serious disease, as there is an opportunity to intervene.
But this type of surveillance is at risk without support and investment. The UK COVID-19 wastewater monitoring programme was wound down earlier this year bowing to budgetary pressures, rather than continuing and pivoting to improve our understanding of other diseases.
The potential of wastewater surveillance has been shown time and again. To realise that potential fully, closer collaboration between researchers, the water industry and policy should be fostered and supported by appropriate funding.
Leon Danon receives funding from UKHSA and UKRI.
Kathleen M O'Reilly receives funding from UKHSA and BMGF.
This article was originally published on The Conversation. Read the original article.







