The Metropolitan Police Commissioner Mark Rowley has announced that the London police force is to attend fewer mental health emergencies. As part of an approach called Right Care, Right Person, police officers will only respond to 999 mental health calls when there is an “immediate threat to life”. The new strategy will be implemented from September 1 2023.
This change has been in motion since Humberside Police created the model in 2020. It is now being adopted by forces across England. In Scotland, a similar reform – Right Care, Right Time – has already been introduced.
Mental health leaders have criticised the move. Adrian James, president of the Royal College of Psychiatrists, said it is “unhelpful and impractical”. Others have accused the police of creating a vacuum, with mental health charity Mind’s Sarah Hughes saying she fears “people will lose their lives”.
But, as my research has shown, that vacuum already exists. Lives are already being lost because of a lack of mental health support in the UK.
For many years now there have been calls, from people both within the police and those experiencing mental health crises, for the police to have less of a role in mental health emergencies. Instead, the police have increasingly been left to pick up the pieces of an overstretched health system.
Under Section 136 of the Mental Health Act, police officers can detain someone if they believe that person’s mental health is causing an immediate risk to the person or others. This legislation can only be used in a public place, which is why detentions fell slightly during national COVID lockdowns.
Emergency response
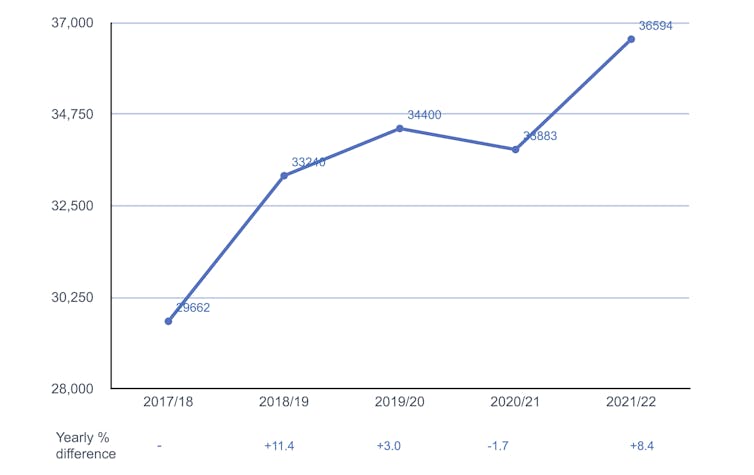
Apart from that small drop in 2020, Home Office data shows that the numbers of people subject to Section 136 detention has risen every year since 2017/18. And in 2021/22, Mind noted that the equivalent of the population of a British town was picked up by the police in this way.
Yearly numbers of Section 136 detentions in England and Wales from 2017/18 to 2021/22:
Scotland’s reform was prompted by similar rising numbers. In 2019 four in every five 999 calls to Police Scotland were reportedly not about crime but vulnerability.
Between 2013 and 2016, my colleagues and I conducted in-depth interviews with 37 people who had been detained under Section 136, as well as with 79 police officers and 160 healthcare staff and volunteers. Working in collaboration with Sussex Police and Sussex Partnership NHS Trust, we were investigating alarmingly high rates of detentions across the county.
Mental health is recognised as a core part of policing. We found, however, that too often the police are the only agency expected to respond to such emergencies, particularly out of hours. As one 18-year old interviewee told us:
[My community mental-health team] are under resourced, and in my most recent meeting with them, I was told that if I’m in crisis, the only option is to call the police.
A traumatic experience
Section 136 is not an arrest where a crime is suspected. People I have interviewed nonetheless describe being detained as degrading and stigmatising. Such accounts have significantly contributed to the introduction of Right Care, Right Person.
The 2017 Policing and Crime Act stopped police custody being used as a place of safety. Police cells were never the right place for someone experiencing a mental health crisis.
Despite this, the lack of provision of alternative places of safety has meant that, rather than handing the care of someone in distress over to a custody sergeant and returning to patrol duties, officers collectively spend close to a million hours a year waiting with patients in hospital settings. This is as humiliating for the people being escorted as it is demoralising for the officers involved.
The idea behind Right Care, Right Person is that people in crisis be cared for by mental health professionals. Since 2013, mental health nurses have joined police officers in street triage schemes, accompanying them on patrol to provide immediate mental health support to people.
Although triage is now widespread and broadly considered helpful, it is not enough on its own. Services must work together, otherwise people will keep falling through the gaps.
Being frequently detained by the police – without proper, long-term mental health support – makes vulnerable people feel worse.
Too often it falls to the police to keep people alive using forceful detention. Those who are being repeatedly detained feel trapped in a dismal cycle that could ultimately end in their death. One person I interviewed, Heather*, put it plainly:
“The police are the only people who have to do something. They can’t leave you. So, I have really mixed feelings on [Section] 136.”
She, like others I spoke to, was not getting the support she needed. Mental health professionals had, in fact, told her that the trauma therapy she needed was not available. She said:
Everything that happens is merely a sticking plaster until the next 136. [Services] know it. I know it. [So] half of me wants some help, the other half wants to be dead.“
Tragically, Heather has since died, as has a brilliant young woman, Liv Pontin, who helped to guide my research and was a powerful advocate for working with the police to improve mental health support.
Research has shown the situations that lead to repeated Section 136 detentions are often rooted in trauma. It is clear that any emergency response has to go hand in hand with long-term support to help address such trauma.
Early in 2023, the Department of Health and Social Care announced extra funding to, as home secretary Suella Braverman put it, "improve the mental health crisis care response”. Time will tell if that is actually enough but long-term support is urgently needed. Too many lives are already being lost.
*All research participants’ names have been changed.
If you’ve been affected by anything in this article and don’t know who to turn to there are free helplines available to support you.
In the UK and Ireland – call Samaritans UK at 116 123.
In the US – call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or IMAlive at 1-800-784-2433.
In Australia – call Lifeline Australia at 13 11 14.
In other countries – visit IASP or Suicide.org to find a helpline in your country.
Claire Warrington has previously received funding from Wellcome Trust and ESRC.
This article was originally published on The Conversation. Read the original article.







