Patients who have lost a significant amount of blood as a result of accident or injury are to be given “whole blood transfusions” in a bid to improve their chances of survival.
Evidence from army medics working in battlefields in Afghanistan suggest that whole blood transfusions could improve survival rates among patients who have suffered a major trauma.
Now the NHS is testing whether such transfusions could help patients who have suffered serious accident or injury in the UK.
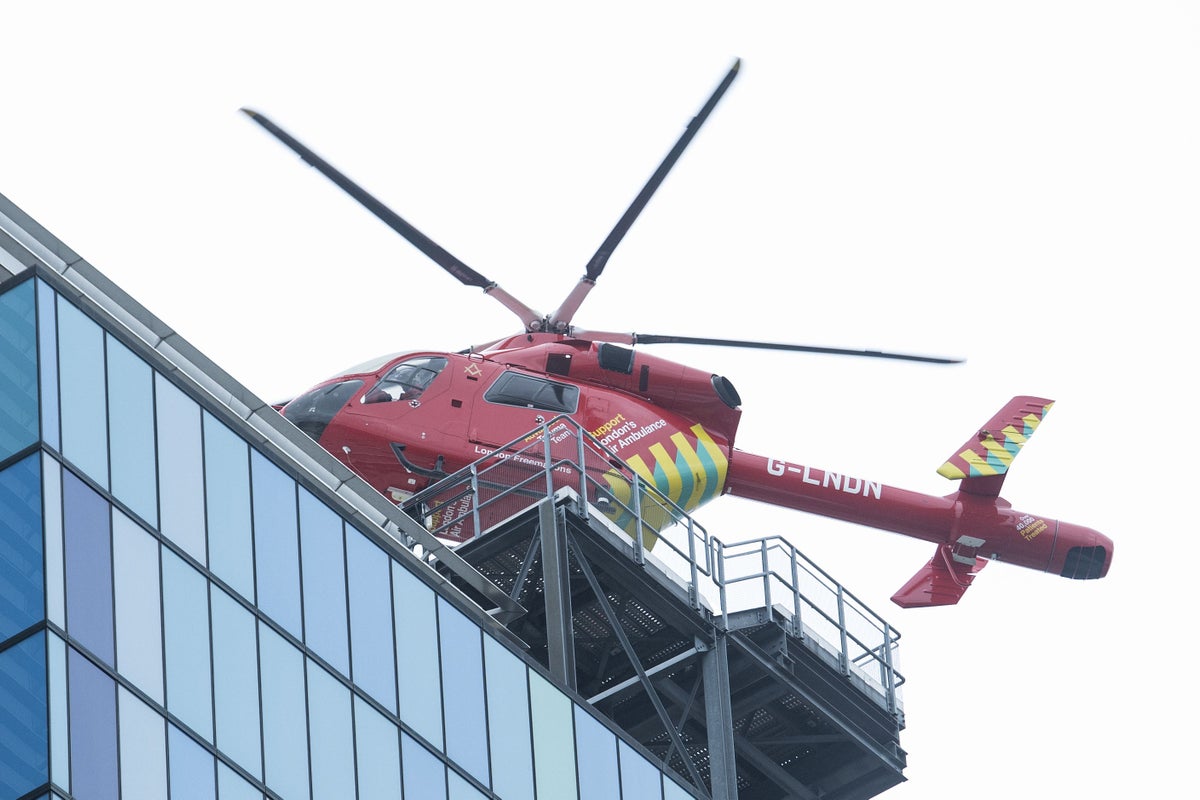
10 air ambulances treating major trauma patients will assess this type of transfusion compared to standard care.
We hope that (the trial) will show there are logistical and procedural benefits in giving a blood transfusion of all of the components in a single bag – and ultimately improved outcomes for patients— Dr Laura Green
Air Ambulance patients, and soldiers needing battlefield transfusions, can receive plasma and red blood cells, but not platelets – all different components of blood.
But the new trial will assess whether giving whole blood transfusions – blood with all the components, just as it would have been coming out of a donors arm – would be a better option.
Experts said that it could cut treatment time compared to transfusing different blood components separately.
Meanwhile platelets in the whole blood donation will help the patient’s blood clot.
Because of the difficulty storing platelets they are not currently used in air ambulances – which usually deal with the most severe injuries or accidents that might require helicopter transport to hospital.
If the trial is a success, it would change pre-hospital trauma transfusions and battlefield care, NHS Blood and transplant (NHSBT) said.
The trial, which will begin tomorrow, starting with London Air Ambulance, has been funded by by NHSBT, the Air Ambulance charities and the Ministry of Defence.
NHSBT said that 848 patients will be recruited for the trial over the next two years with half receiving usual care and the other half to get whole blood transfusions – which will come from donors with 0 negative blood – the universal blood type.
“The role of air ambulances in providing blood transfusions at the scene of an incident is crucial – delivering the most challenging treatments in the most challenging environments,” said Dr Laura Green, co-chief investigator for the trial and consultant in haemostasis and transfusion Medicine at NHS Blood and Transplant.
“Any delay to starting transfusion during traumatic blood loss can reduce the chances of survival.
“We hope that (the trial) will show there are logistical and procedural benefits in giving a blood transfusion of all of the components in a single bag – and ultimately improved outcomes for patients.
“We are also incredibly grateful to our O Rh negative donors, whose universal donor blood is critical in trauma transfusion – including in this trial.”
Professor Jason Smith, co-chief investigator, from the Ministry of Defence, said: “We have known that blood transfusions save lives in patients with life-threatening haemorrhage for over 100 years, but the exact nature and optimal timing of those transfusions is still not known.
“This study will hopefully give us the answer as to whether whole blood is better than our current standard care in terms of clinical and cost effectiveness.
“Whole blood contains platelets. The only way to transfuse platelets in the pre-hospital setting is through whole blood. There is evidence there may be a benefit to giving patients platelets as close as possible to the point of injury.”