Hospitals have issued an urgent warning as flu cases continue to soar across the UK.
Patients have been urged to attend A&E alone as NHS hospitals grapple with high demand.
Some have also restricted visitor numbers while others are encouraging people to wear surgical masks to limit the spread.
Several NHS trusts have declared critical incidents due to “exceptionally high demands” in emergency departments, with a patient at one hospital forced to wait 50 hours to be admitted to a ward.
Around 5,000 hospital beds in England are occupied with patients with flu.
York and Scarborough hospitals asked for public support by asking patients to seek medical attention alone where possible.
Dr Ed Smith, deputy medical director at York and Scarborough Teaching Hospitals NHS Foundation Trust, said: “Our emergency departments are busy all year round but are exceptionally busy at the moment with a high volume of poorly patients attending.
“This means that the departments can often be overcrowded, with limited places to sit while waiting to be seen.
“While we understand it’s appropriate for a friend or family member to accompany with a child or as a carer for example, if patients can attend alone, this will help free up much-needed space for other patients.”
North Bristol NHS Trust, which runs Southmead Hospital, urged both the public and staff to wear surgical face masks in its “emergency zone”.
(1/4) In common with NHS organisations across the country, NBT has seen a sharp rise in flu and respiratory illness over the last few weeks – and in particular since the start of January. pic.twitter.com/AfbnpMlg7w
— North Bristol NHS Trust (@NorthBristolNHS) January 7, 2025
It said: “This is to reduce the risk of infection and to enhance the safety of all concerned.”
Meanwhile, East Sussex Hospitals Trust announced on Tuesday it is temporarily limiting visiting to one visitor per patient per day to reduce the impact of flu.
“Exemptions apply to end-of-life care, our special care baby unit and when visiting children under 16,” a statement said.
“Additional visitors will be permitted on compassionate grounds on a case-by-case basis for all of our other services.”
📢Due to sustained pressures at our Basingstoke and Winchester hospitals, we have declared a critical incident.
— Hampshire Hospitals (@HHFTnhs) January 7, 2025
Our emergency departments are facing extremely high attendance levels. Non-life-threatening conditions will result in long waits. pic.twitter.com/CBBUJyEHV9
Hospitals in Northamptonshire, Cornwall, Liverpool, Hampshire, Birmingham and Plymouth have all declared critical incidents in recent days.
East Midlands Ambulance Service NHS Trust also declared the first critical incident in its history due to a combination of “significant patient demand, pressure within local hospitals and flooding”.
Critical incidents can be declared when health and care services are so busy that special measures are needed to restore normal operations and keep patients safe.
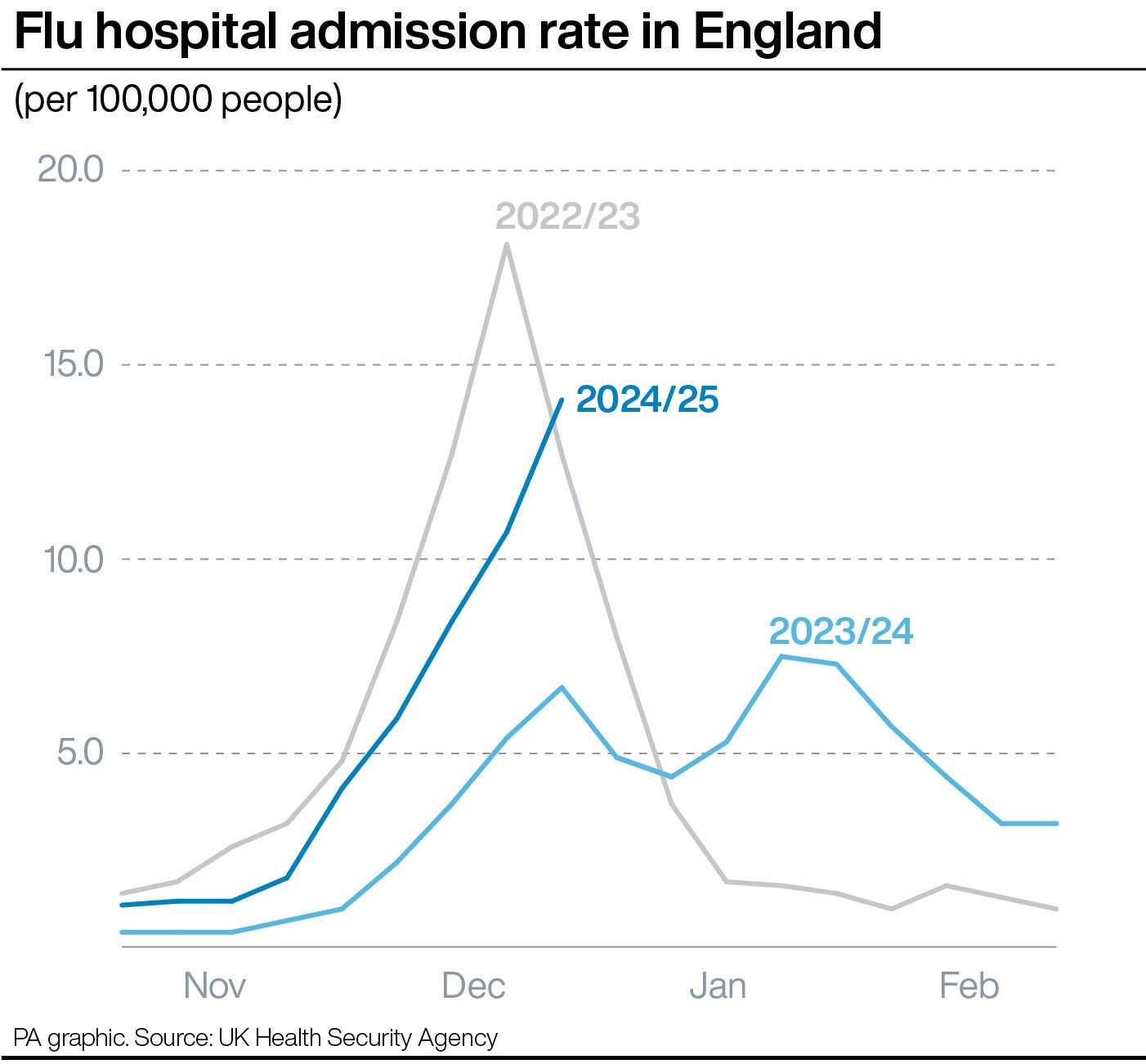
Last week, NHS data revealed the number of people in hospital with flu in England was more than four times the level it was a month ago, with officials warning cases are “rising at a very concerning rate”.
It is expected that data released later this week will show another rise in the number of people admitted to hospital due to flu.
On Wednesday, Saffron Cordery, interim chief executive of NHS Providers, said working conditions for staff are “incredibly difficult” owing to inadequate NHS buildings with not enough room for patients.
She told BBC Radio 4’s Today programme the NHS is under pressure and flu is currently 246% higher than last year.
“What we’re also seeing is this challenge of flow of patients through the system and increasing demand, which has led to these critical incidents being declared across a number of trusts, and uniquely, actually across ambulance services as well,” she said.
“We haven’t seen that before, which really speaks to that level of demand.”

She urged patients who are suffering a life-threatening emergency to still call 999.
Annie Farrell, a GP in south Liverpool and chairwoman of the Liverpool local medical committee representing GPs, said there is “increasing virus overload in patients, increasing frailty in our patients, the numbers of patients that aren’t able to self-care for these kinds of conditions is going up”.
She added: “For quite a while now, we know as a GP that if we feel somebody needs to go to hospital, we’re having to sit down with them and say we’re sentencing you to potentially over 24 hours in a plastic chair in a waiting room.
“There will be care available – I know for a fact that our A&E department are doing their absolute best to manage everybody who is waiting for a bed in hospital in whatever circumstances they find themselves, so some of them are in backs of ambulances, and some of them are in the waiting area, but that’s what we’re faced with.”
NHS England’s national medical director, Professor Sir Stephen Powis, said: “Frontline NHS staff are under significant pressure and the demand is showing no signs of letting up, with latest data showing flu cases skyrocketed to around 5,000 a day in hospitals at the end of last year and multiple trusts across the country declaring incidents to help them to manage additional strain on services.”