Pre-planned specialist care is “no longer fit for purpose” and needs to be reformed, leading medics have said.
The Royal College of Physicians (RCP) said that the current outpatient care service in the NHS – which includes pre-planned tests or investigations, treatments and consultations with specialist medics – is “ineffective for both patients and staff”.
A new report by the College and the Patients Association, says that reforming outpatient care will be an “essential” part of the Government’s aim to shift care from hospital to the community.
The current approach to outpatient care often results in long waits; follow up appointments “not aligned to patient need”; so-called “low value” appointments and patients experiencing difficulty navigating services, the report states.
It adds that outpatient care is “largely delivered through appointments at routine intervals” with 135.4 million appointments taking place in England in 2023/24.
But these appointments were “often associated” with delays, poor communication, and confusion caused by trying to navigate services.
The authors of the report said that care must be transformed to give patients more “timely, productive and personalised care”.
They said that the Government’s upcoming 10 Year Plan for health is an opportunity to reform the system.
The new report sets out 40 recommendations to improve care.
Have your say and share the ideas you have for change.
— NHS England (@NHSEngland) October 21, 2024
Help us shape the future of the NHS. ➡️ https://t.co/bm6WSqEupu pic.twitter.com/E7F61ClCMP
“NHS outpatient care is fundamentally no longer fit for purpose,” said Dr Theresa Barnes, RCP clinical lead for outpatients.
“It is archaic, disjointed and ultimately ineffective for both patients and staff.
“It has remained largely unchanged for decades, despite advances in technology.
“Most people on NHS waiting lists are waiting for an outpatient appointment, patient care is increasingly complex, and the medical workforce is frustrated and desperate for change.”
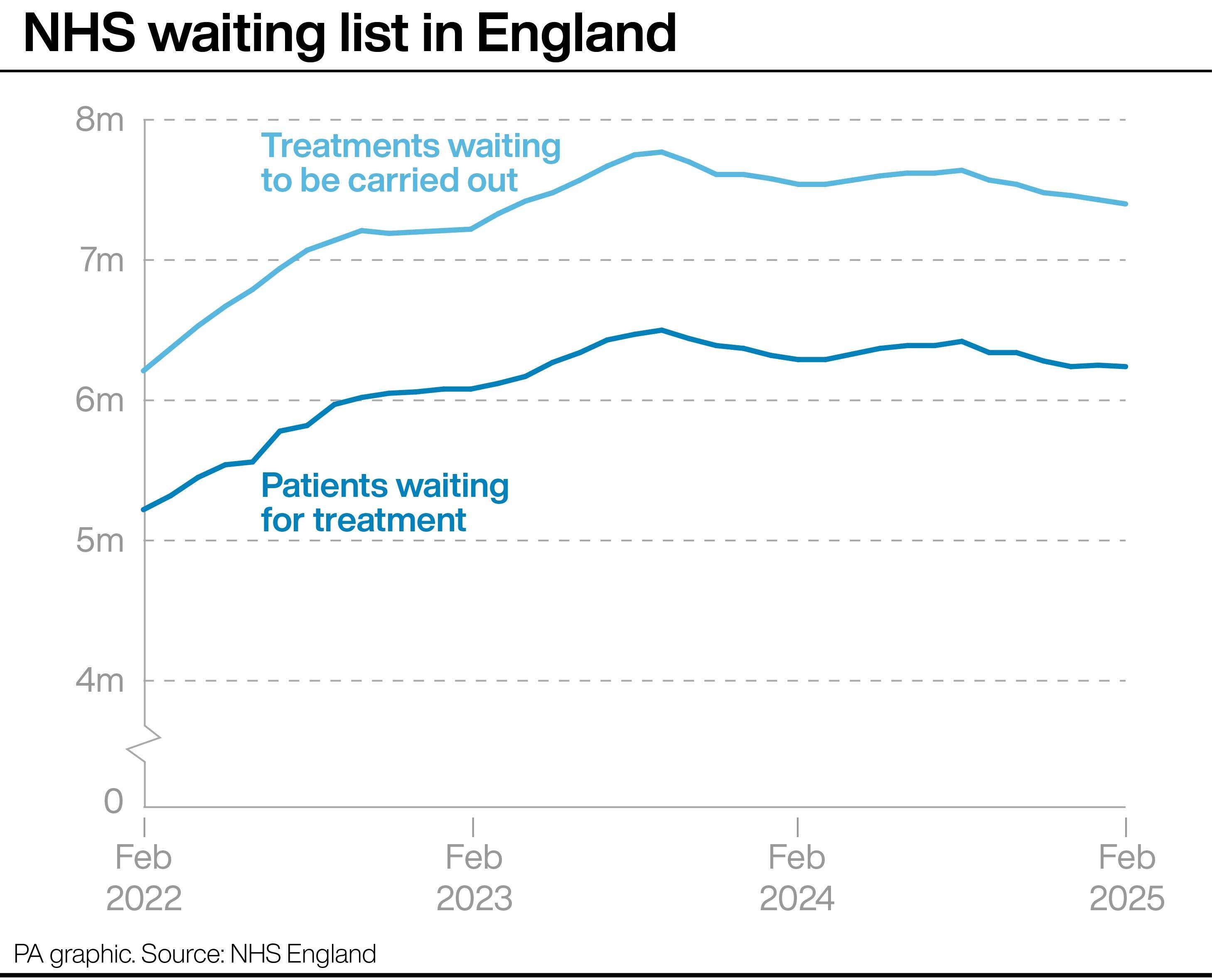
The latest NHS figures for England show that an estimated 7.4 million treatments were waiting to be carried out at the end of February, relating to 6.24 million patients.
This is down from 7.43 million treatments and 6.25 million patients at the end of January.
Dr Barnes added: “Our new report draws on the ideas and expertise of doctors and patients to embrace a new way of doing things – prioritising people, rather than the system.
“We need a significant shift in the way we deliver planned specialist care.
“Getting this right is integral to bringing down NHS waiting lists and delivering the Government’s three shifts. Now is the time to be radical.”
Rachel Power, chief executive of the Patients Association, added: “Too many patients tell us that outpatient care feels like an uphill battle, with delays, confusion, and a lack of joined-up communication that leaves them feeling powerless.
“Planned specialist care must be built around the needs of real people, not rigid systems.
“With the upcoming implementation of the 10-year health plan, the use of technology to improve access, reduce inequalities, and support people to manage their own care is vital.”
The RCP has called on the Government to expand the specialist workforce, increase medical school and postgraduate training and said that doctors should be supported with appropriate administrative support and digital infrastructure.
A Department for Health and Social Care spokesperson said: “Our 10-Year health plan will fix the broken outpatient system – shifting more care to the community so patients can be seen in the right setting, and moving the NHS from analogue to digital to tackle poor communication and delays.
“We have already made progress on our mission to cut waiting lists – delivering an extra 3 million appointments and cutting the waiting list by 219,000 since July.”