Insurers and healthcare middlemen are making it harder for everyday Americans, including many living with chronic diseases, to access the prescription drugs they need.
Fortunately, Congress and President Joe Biden can address the problem by passing two bipartisan reforms during the current "lame duck" legislative session. For Democrats, this is a chance to build on the historic progress already made toward healthcare access and affordability for all Americans.
At issue are middlemen known as "pharmacy benefit managers" -- or PBMs. PBMs act on behalf of insurance companies to negotiate with drug manufacturers and administer "formularies," or lists of which medications the insurer covers and what patients owe out of pocket.
PBMs use their control over formularies to extract price concessions from drug companies in the form of rebates and discounts. Since drug makers want their products to be covered by insurers, they have a strong incentive to comply with PBMs' demands. In 2023 alone, the total value of rebates, discounts, and other payments to PBMs and insurers may have been as high as $334 billion.
These savings could meaningfully reduce prescription drug costs for millions of patients. But in practice, many health plans simply keep rebates and discounts for themselves while continuing to charge patients based on the nominal "list price" of a drug, rather than the much lower "net price," which accounts for discounts and rebates.
Consider a privately insured patient with diabetes. Let's assume the list price of the insulin she needs to survive is $1,000 per month, and her plan's coinsurance obligation is 25%. Let's also assume her insurer/PBM negotiates a 75% rebate off the insulin's price -- a 70-80% rebate is standard for many insulin brands. That'd leave the insurer/PBM paying a "net price" of $250 for the drug.
But under current rules, the patient's health plan could still charge her based on the $1,000 per month list price of the insulin, meaning she'd owe $250 at the pharmacy counter. In this scenario, the sick patient would be covering 100% of what her health plan paid for the medicine. That isn't how insurance is supposed to work.
This hypothetical example is no outlier. It's the reality for thousands of Americans with diabetes. One study found that people with diabetes could save $3.7 billion per year on their medications if insurers and PBMs passed rebates and discounts through to patients.
A more fundamental issue is that in today's distorted market, PBM compensation is directly tied to how much medicines cost. The rebates, discounts, and fees PBMs collect are typically calculated as a percentage of a drug's list price. Since PBMs get to keep a portion of these payments for themselves, they naturally gravitate toward the most expensive drugs.
While this setup works well for PBMs, it harms patients. Because PBMs make more money on expensive medicines, they're incentivized to select the costliest drugs for insurance plan coverage, even when cheaper alternatives exist. Over time, this inevitably leads to higher patient costs at the pharmacy counter.
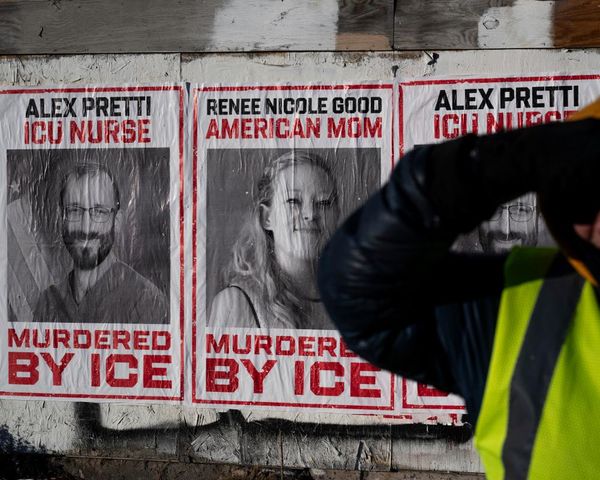
PBM practices hit the 129 million Americans living with heart disease, cancer, diabetes, and other chronic illnesses particularly hard. Around half of patients living with chronic diseases already skip doses or forgo treatment for cost reasons -- much higher than the overall rate of medication "nonadherence" among all adults.
When patients don't take their medications as directed, whether it's because of cost or other reasons, manageable conditions can snowball into costly and life-threatening emergencies. By refusing to pass savings along to patients and pushing people toward the most expensive drugs, PBMs and insurers could be inadvertently making the problem of non-adherence worse.
The good news is that Congress seems to be waking up to this reality. Two bipartisan reforms have been gathering momentum in recent months. One bill would delink PBM compensation from drug prices and the other would require health plans and PBMs to share rebates and discounts with patients. Both bills have already passed the Senate Finance Committee.
For Democrats, this is a chance to demonstrate our commitment to equitable and affordable health care. PBM reform would help ensure our most vulnerable citizens, already reckoning with a cost of living crisis, aren't forced to choose between medication and other necessities. It's also an opportunity to build on Democrats' recent work to advance healthcare affordability through the Inflation Reduction Act and other legislation.
But this isn't just a Democratic issue. A recent poll revealed that nearly two-thirds of voters would favor candidates who pass such legislation. PBM reform is that elusive combination of good policy and smart politics.
PBM reform is a golden opportunity for Congress to deliver on a critical kitchen-table issue that impacts millions of Americans. Let's hope they take it.
Kenneth E. Thorpe is the Robert W. Woodruff Professor of Health Policy at Emory University and the chairman of the Partnership to Fight Chronic Disease.