Congress poured money into the U.S. economy throughout the COVID-19 pandemic. But for a few hospitals, one of the lifelines that Medicare threw to the medical industry ultimately became another stone around their necks.
Medicare flooded hospitals with cash after the virus prompted the Trump administration to halt elective care — a crucial source of revenue — but not all of that money was a giveaway. In fact, $107.3 billion came through advances on Medicare claims that were doled out between April and October of 2020.
Three years later, some medical providers are still struggling to pay it back.
A Mississippi hospital’s debt was a factor in its failed bid to be acquired by a major academic system. And it’s one of the underlying reasons a rural Arkansas health system is looking to sell its real estate.
While the relief money was generally enough to account for the steep drop in revenue and skyrocketing costs, hospitals were unprepared for the time it would take for the economy to recover, according to Ge Bai, an accounting and health policy professor at Johns Hopkins University.
When the Centers for Medicare and Medicaid Services announced the program, Bai thought it was another great way to funnel aid to hospitals. In hindsight, she said, the advances should only have been used as a last resort.
“But they spent it,” she said.
Just a fraction of the money — around $404 million, or 0.37 percent — is still outstanding, and is therefore not considered a widespread problem by regulators or rural health associations. No one is rushing to the hospitals’ aid, but for some rural facilities, the extra debt is now contributing to their ongoing struggle for survival.
Keeping the advance as a reserve fund was also easier said than done. Labor and supply costs surged during the pandemic, and while they are starting to decline, hospitals face ongoing drug shortages and increases in uncompensated care as states revisit eligibility for Medicaid enrollees. The gap between better and worse performing hospitals is widening, according to hospital consulting firm Kaufman Hall.
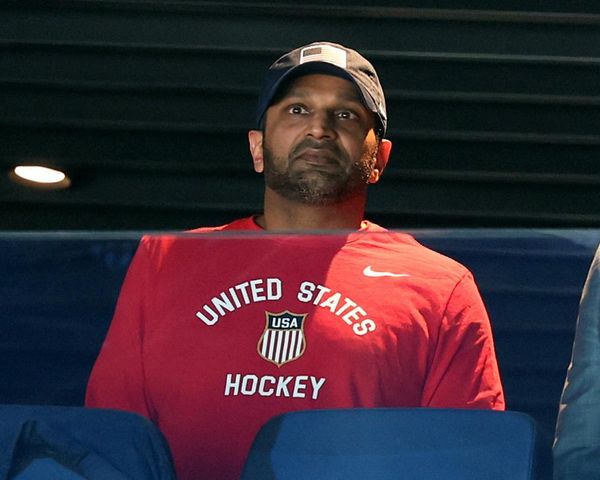
Paul Taylor, CEO of the private Ozarks Community Hospital, headquartered in Gravette, Ark., said his pleas to rural health associations went unheeded.
“There just weren’t enough voices clamoring for help,” he said.
The health system, which includes the main hospital in Gravette along with 16 clinics scattered throughout Arkansas and Missouri, should have filed for Chapter 11 bankruptcy last year, Taylor said.
“But we’re stubborn.”
Advance payment program
A March 2020 COVID-19 aid law expanded an existing Medicare program that advances funds to medical providers in need. The COVID-19 Accelerated and Advance Payment, or CAAP, program, calculated advances to health care organizations by size and designation beginning that April.
The program was halted in October, and repayment terms were made more flexible, but not as flexible as some lawmakers in Congress proposed. The Centers for Medicare and Medicaid Services deferred the debt for one year, then began recouping payments by taking 25 percent off billed claims for 11 months, increasing to 50 percent for the following six months.
After that, the agency demanded repayment in full unless hospitals qualified for a long-term hardship plan at 4 percent interest.
The struggle for some hospitals to pay off the debt illustrates the financial complexity they face once they go underwater.
Taylor said he “begged, borrowed and stole” to keep the doors open. Ozarks filed for an employee retention tax credit to offset part of the CMS recoupments. But an unexpected dispute over the repayment time frame lengthened the 50 percent recoupment for another six months.
A CMS spokesperson said the recoupment timeline for Ozarks was “in-line with the phased recoupment schedule Congress outlined.”
Arkansas lawmakers intervened with CMS on Ozarks’ behalf. But it wasn’t until Taylor had a conversation with senior CMS officials and secured a separate bank loan that the hospital qualified for a five-year hardship repayment plan last November.
“Rural hospitals are critical to the delivery of healthcare in Arkansas and we’re committed to ensuring they have the resources to continue serving the local community,” Sen. John Boozman, R-Ark., said in a statement. “I’m pleased we were able to help facilitate flexibility for Ozark Community Hospital so it can continue providing quality care citizens depend on.”
Ozarks still has around $3 million in debt out of an initial $9.6 million received from the program, and is $27 million in debt overall.
Revenues recently began reaching pre-pandemic levels, Taylor said, but inflated labor and supply costs are still above pre-pandemic levels. When the state slowed an expected grant program by implementing additional accountability measures, Taylor initiated “plan Z” — selling the hospital’s real estate.
The sale would cut Ozarks’ debt from $27 million to $10 million, he said, though he knows that selling the land will cost him more in the long run.
“Those guys don’t make investments like that that they don’t plan on profiting from,” he said of real estate companies. “It is what it is, and you do what you have to do, and it will continue to be a cash flow consequence for the next 20 years.”
Greenwood Leflore Hospital, a public facility in Greenwood, Miss., still owes $4.7 million of its $16.5 million advance, according to spokesperson Christine Hemphill. The hospital started a five-year payment plan in October 2022 and won’t finish paying it off until September 2027.
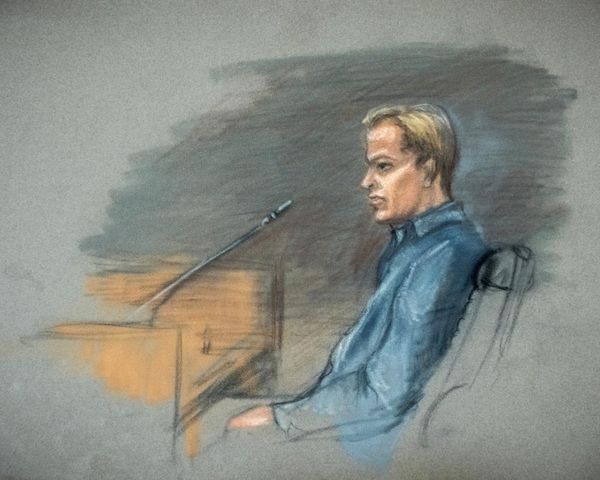
The hospital’s debts were a major reason a pending deal to merge with the University of Mississippi Medical Center fell through, even after interim CEO Gary Marchand secured a line of credit to help insulate UMMC from the financial burden.
The hospital started cutting services earlier than it otherwise would have once the recoupments started, Marchand said. Initial gratitude gave way to stress as the debts piled up, and Marchand hoped “the cavalry would come” to forgive the advance for hardship reasons. But the statute didn’t allow for any wiggle room.
“The cavalry never showed up,” he said.
Greenwood is also waiting to hear back on an application for critical access status — a designation that applies to Ozarks — which would grant the hospital a 1 percent bonus on Medicare claims. The hospital is likely to close if the application is rejected.
“We just don’t see any other way,” Marchand said.
Long-term solutions for rural hospitals need to contend with the reality of declining rural populations, Bai said, which translates to lower revenues. Taxpayers are often stuck footing an ever-growing share of the bill.
A new designation under Medicare allowing hospitals to focus on emergency and outpatient care went live this year, and a number of small rural hospitals are already converting. Similar options might be a better alternative to sustain access to care in rural areas, she said.
Both Ozarks and Greenwood Leflore are around 30 minutes away from the next nearest hospital.
“We have to hit a balance,” Bai said, “between convenience and financial viability.”
(This story is part of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund.)
The post Medicare pandemic advances deepen debt for some hospitals appeared first on Roll Call.