One in every 100 deaths globally is by suicide. Each year, more than 700,000 people die by suicide. A staggering 77% of suicides occur in low- and middle-income countries, with the African region bearing the highest burden at a rate of 11.2 deaths per 100,000 people. In Kenya, the crude suicide rate is 6.1 deaths per 100,000 people. Men are three times more likely to die by suicide than women. Linnet Ongeri is a psychiatrist and a mental health researcher with a focus on suicide prevention. She examines the factors behind Kenya’s suicide rate and recent efforts to decriminalise attempted suicide.
What are the drivers of suicide?
Suicide is a complex issue. It results from the interplay of various factors, including genetic, biological, psychological, socioeconomic and cultural influences.
There is a strong link between suicide and mental health disorders. However, many suicides occur impulsively during moments of crisis or in response to significant life challenges. These challenges often involve the denial of basic human rights and access to resources. They could also be brought on by stressful events like a loss of livelihood, academic or work-related pressures, relationship breakdowns and other life crises.
Stigmatising views portray suicide as a sign of weakness or failure, rather than a result of deep emotional distress or mental health challenges. Suicide stigma refers to the negative attitudes, beliefs and misconceptions that surround individuals who experience suicidal thoughts or attempt suicide. This stigma often manifests as judgment, shame or social exclusion. This makes it difficult for people to openly discuss their struggles or seek help.
Societal stigma isolates individuals and creates barriers to accessing mental health support. This further compounds the risk of suicide.
What role does the criminalisation of suicide play?
The relationship between stigma and the criminalisation of suicide is especially concerning.
In Kenya, Section 226 of the penal code states that any person who tries to kill him or herself is guilty of a misdemeanour. He or she is liable to imprisonment of up to two years, a fine, or both. This law, inherited from the English common law, has been repealed in several countries globally.
Suicide was criminalised under British law prior to the 1960s largely due to historical and religious beliefs. These beliefs viewed suicide as a moral transgression and influenced legal systems. In 1961, efforts to decriminalise suicide gained global momentum following growing recognition of the link to mental health. Of the 20 countries that still criminalise attempted suicide, nine are in Africa.
Even though the law is aimed at deterring people from taking their own lives, there is local and international evidence that criminalisation of attempted suicide increases suicide risk. Treating survivors of suicide as criminals worsens the stigma that surrounds mental health. This impedes them from seeking help and support.
The threat of legal sanctions for a suicide survivor, who is already experiencing severe mental anguish and emotional distress, can have serious negative repercussions. Punitive measures can worsen an individual’s mental health, increase their sense of isolation and make them more vulnerable. This heightens the risk of suicidal behaviour.
Further, criminalisation of suicide impedes accurate data collection and prevention-related interventions. A clearer understanding of who is affected and why is critical for designing context-specific prevention strategies that use limited resources effectively.
Kenya has made progress in developing a national suicide prevention strategy. However, several of its proposed interventions are at odds with the existing legal framework.
This legal incompatibility hinders the government and healthcare providers from carrying out the strategy.
Why is decriminalising suicide important?
Decriminalising suicide safeguards individuals’ right to health by enabling them to seek care and support during times of crisis.
It helps shift the narrative from treating attempted suicide as a criminal act to recognising it as a mental health crisis. This reduces stigma and encourages open discussions about mental health. Healthcare providers can focus on offering treatment rather than involving law enforcement. It also allows survivors to get help without fear of legal consequences or discrimination.
Both the United Nations Sustainable Development Goals and the World Health Organization’s (WHO) Comprehensive Mental Health Action Plan aim to reduce the global suicide rate by one-third by 2030.
As a WHO member state, Kenya is committed to achieving this target. Kenya’s suicide prevention strategy aims to reduce suicide deaths by 10% by 2026.
What’s being done to decriminalise attempted suicide in Kenya?
A 2020 report from a national task force on mental health emphasised the need to decriminalise attempted suicide. It also called for a national suicide registry to improve access to mental healthcare, suicide crisis support, and data on suicide and suicidal attempts. These recommendations would support the country’s suicide prevention strategy.
In 2022, the Kenya National Commission on Human Rights filed a constitutional petition to repeal Section 226 of the penal code, deeming it unconstitutional. The petition argues that the current law violates the rights of individuals living with mental health conditions. A final judgment on this case is expected in November 2024. It would be a crucial step towards aligning Kenya’s legal framework with mental health advocacy and human rights.
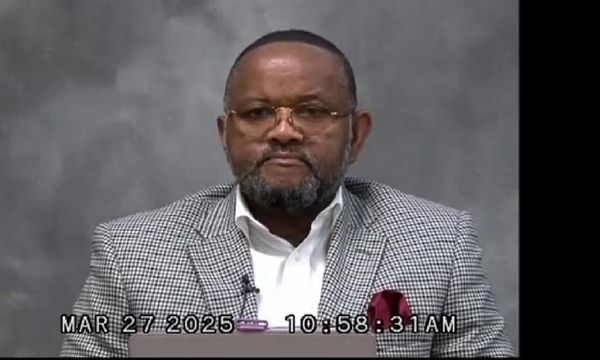
In August 2024, Lukoye Atwoli, an associate director of the Brain and Mind Institute at Kenya’s Aga Khan University, launched a petition with the national assembly calling for the decriminalisation of attempted suicide.
These efforts reflect a growing recognition of the need to address suicide as a public health issue rather than a criminal offence.
What needs to happen next?
Lessons from countries like Ghana and Pakistan, which recently decriminalised suicide, emphasise the need for continued advocacy and awareness.
A key next step is to develop an awareness programme to ensure that the shift in law (when it does happen) is accompanied by meaningful changes in practice.
This programme should focus on training first responders – including police officers, emergency healthcare providers, mental health professionals and peer supporters – who interact with individuals at risk of suicide. Proper training will equip them with the skills to offer compassionate support, timely intervention and appropriate care. This would help ensure decriminalisation efforts translate into tangible improvements in suicide prevention and mental health care.
Linnet Ongeri does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.