For over 50 years, psychiatrists focused on dopamine and serotonin pathways for antidepressant treatment. Since the discovery of the antidepressant effects of ketamine roughly 25 years ago, psychiatrists appreciated that depression could also be treated with great efficacy by targeting the glutamate pathway, the main highway for information in the cerebral cortex and a chemical key to learning and memory.
Recent research using brain scans to measure brain structure and function indicate that the glutamate system also “suffers” from depression, with reduced synaptic connections between nerve cells and reduced efficiency of communication between nerve cells. These changes alter the ability of the brain to regulate emotion, process pleasurable experiences, and think clearly; symptoms commonly associated with depression.
Remarkably, one way to target the brain changes associated with depression is the 1960s anaesthetic, animal tranquiliser, and recreational drug, ketamine. It's now at the forefront of a revolution in depression medication.
A long-term study conducted by Johnson and Johnson in which over 1000 patients were treated with the related drug, Esketamine (one of the two mirror image molecules comprising ketamine) for, on average, 42 months recently reported results. They found that, compared to standard antidepressant treatments, Esketamine reduced the risk for suicide attempts by approximately ten-fold and risk for suicide death by five-fold.
More remarkably still, Esketamine also cut all-cause mortality risk by two-thirds: a reminder that depression isn't just about emotional pain but is a whole-body disease that can reduce lifespan by a decade.

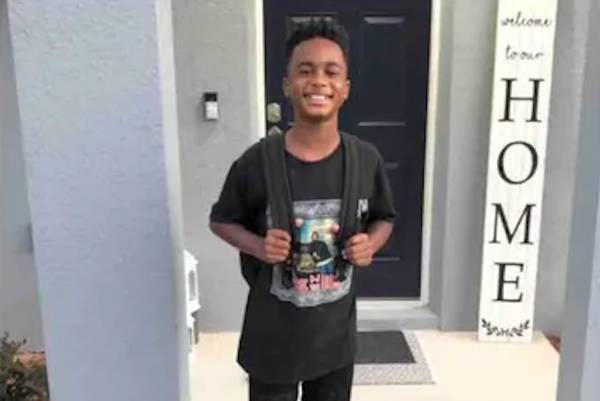
Administered at low doses (0.1 mg/kg), ketamine acts like a mild anxiolytic – similar to a glass of wine. At the therapeutic dose (0.5 mg/kg), it has remarkable antidepressant effects. But push it to 2.0 mg/kg, and you get anaesthesia without antidepressant benefits. This narrow therapeutic window means professional administration is crucial – recreational use or unsupervised home treatment can lead to devastating consequences, as we saw with Matthew Perry.
The treatment itself is straightforward: ketamine is administered intravenously at 0.5 mg/kg over forty minutes, with sessions lasting about two hours. Treatment typically begins with twice-weekly sessions for the first month before decreasing to weekly. Many patients eventually transition to treatments every other week, and some can reduce frequency even further while maintaining benefits.
So why aren't more patients receiving this breakthrough treatment? The answer lies in both infrastructure and attitude. Many practitioners and patients simply aren't aware of ketamine's proven superiority over alternatives. Additionally, ketamine treatment requires specific resources: IV administration capabilities, recovery spaces, and blood pressure monitoring equipment.
There side effects too, including nausea, vomiting, and dissociative symptoms. This has led to the emergence of "Interventional Psychiatry" – specialised practices equipped to deliver these intensive treatments. But we need more facilities like these to meet a growing demand.

Ketamine is heralding a new era in psychiatric treatment, along with psilocybin (in late-stage FDA review for depression) and MDMA (currently being evaluated for treatment). The evidence is clear: we have a powerful tool for fighting depression that works better and faster than traditional treatments.
The challenge now is not to prove ketamine's effectiveness but to ensure this breakthrough reaches the patients who need it and that it is delivered in ways that ensures effectiveness and patient safety.