Sitting at his dining room table, Kelsey Klausmeyer, 41, looks at a picture of his late husband, Enrique Klausmeyer-Garcia, known to most as Ricky. He died almost exactly a year ago, at the age of 37.
Kelsey can’t make sense of it.
When they met, Kelsey was awed by Ricky’s story: his long battle with addiction, his years of sobriety, his advocacy for recovery.
Now, after his death and in the midst of a nationwide addiction crisis, the narrative around Ricky’s life is less tidy.
Ricky is the inspiration for a Washington state law – known as Ricky’s law – passed in 2017 that enables loved ones and public safety officials to compel people experiencing substance abuse to undergo treatment, even if they are unable or unwilling to do it themselves.
The US has been experimenting with these forced-commitment laws for decades. The debate over their efficacy, practicality and ethicality is seeing renewed urgency in states such as New York, California and Washington, where addiction and severe mental health disorders have become a highly visible and highly political issue.
Ricky’s story brings into sharp relief one of the fundamental and difficult questions that officials in these places are grappling with: to what extent should society override an individual’s rights in the name of saving their life and protecting public safety?
For Kelsey, Ricky’s story is not primarily about public policy. It’s a story of immense personal joy and loss, laid before him in a handful of pictures. Here they are with their dog, Otis, whom Ricky “treated like our child”, chuckles Kelsey. Here they are in 2022 on their wedding day, both smiling, fit and handsome at a sunny mountain resort 90 minutes from their home in Seattle. Two hundred of their friends and family came to spend three days celebrating.
Here is Ricky with members of his sprawling family. When the couple first started dating, they discovered, remarkably, that they were both from families of nine siblings, both raised Catholic. “We always thought we were kind of destined in a way,” says Kelsey.
Kelsey grew up in Kansas; Ricky’s family immigrated from Mexico. They met online. Ricky was direct about what he wanted, a quality Kelsey, a naturopathic doctor, found attractive. “He shared that his dream was to have a family, to have kids, have a dog, have a house, have a husband,” remembers Kelsey. Those were prizes neither of them had felt certain were winnable. Together, they brought that picture into focus.
In those early, heady weeks of dating, Ricky was candid with Kelsey about his history with substance use disorder and his journey of recovery. Kelsey was undaunted.
“I just thought so highly of that, for somebody to have suffered with that disease as much as Ricky did, and then to turn around and do something for the greater good like he did,” remembers Kelsey. “That got me. That was the moment I fell in love with Ricky.”
But within the first year of their marriage, and despite Kelsey’s relentless attempts to help him, Ricky would be gone.
Seventy-five hospital visits, and increasing desperation
With his good looks, his authenticity, his goofy enthusiasm for life and willingness to be vulnerable, Ricky was a charmer. Kelsey wasn’t the first person to fall for him.
More than a decade before he met his future husband, Ricky met Lauren Davis. Their friendship would become one of the most important relationships in his life, and the driving force behind the involuntary-commitment law created in his name.
The two were in their late teens in 2004, working as assistant preschool teachers in Redmond, Washington. “I had an enormous crush on Ricky and spent several failed years attempting to woo him,” says Davis of their early friendship. Once they’d established she wasn’t his type, Davis became his “wing woman” and accompanied him to gay clubs. “I’m a white girl who grew up in Washington,” she says. “I can’t dance to save my life, but I sure tried.”
In the next few years, as the two grew into young adults, Davis would become a different kind of wing woman for her friend. Ricky spiraled into a serious problem with alcohol and occasional opioids. “I knew I was feeling depressed,” he recalled years later, in a public radio interview with the Seattle station KNKX. “I was feeling really anxious; most of the time I just wanted to escape all that. I just started to self-medicate and take whatever it took to escape reality.”
The first time Davis called 911 and had her friend taken to the hospital, she remembers his blood alcohol was dangerously high – she would find out it was at a near fatal level. He was admitted to the hospital’s psychiatric unit. Davis sat with him in his room from 8am to 8pm. She described trying to leave Ricky’s hospital room, “hugging him and he wouldn’t let me go”.
This episode set off a corrosive cycle of hospitalization, brief sobriety and relapse. Eventually, Ricky became suicidal.
“I found myself consistently in a position of trying to catch him, before he died, essentially,” says Davis. “In the course of those two years, he was in the emergency department over 75 times. I was at his bedside for most of those visits.” Numerous doctors told her to plan for his funeral. Davis refused. She would not stand by and watch her friend die.
Ricky’s father had terminal cancer during this period and despite family members’ efforts to help Ricky, his addiction stressed relationships. Davis became his primary advocate and champion.
Watching Ricky’s struggle, Davis was horrified at how little she could do to help him. What she wanted was to put her friend into an addiction treatment facility, because he was too sick to do it himself.
But at that time, in 2011, Washington law only allowed for involuntary commitment based on a psychiatric diagnosis, not for a substance abuse disorder. Other states had more expansive criteria.
Davis remembers Ricky on his sixth psychiatric hospitalization. “He had this young psychiatrist who looked across at him and said, ‘You know, if we were in another state and I could involuntarily commit you for your addiction, I would.’”
But in Washington state, the doctor said, “his hands were tied”.
A contentious history
American public policy has grappled with the concept of involuntary commitment since at least the 1850s. As many as 14 states had laws on the books before the turn of the 20th century allowing for civil commitment for “habitual drunkenness”. Often, offenders would be locked in asylums.
Over time, enthusiasm for this approach began to fade “because of the lack of evidence that the facilities were really able to cure substance abuse”, says psychiatrist and historian Paul Appelbaum, who teaches at Columbia University and studies medicine and ethics. Legislators – and the public – stopped supporting the investment. The country saw another wave of these statutes in the 1960s. Today, though roughly two-thirds of states have civil commitment laws that specifically include substance use, many are rarely used.
In part, that’s because there is still little consensus about the efficacy of committing someone to treatment against their will. “There are almost no data indicating whether it works or for whom it works,” says Appelbaum. Policymakers, he says – chronically guilty of short-term thinking – have been reluctant to invest in meaningful efforts to evaluate these kinds of programs. Those that have tried have shown mixed outcomes, and they often don’t measure long-term results.
Many who study addiction and substance use have ethical concerns. Holding someone long enough for treatment to possibly be effective, say some, is immoral.
Dr Liz Frye, who practices addiction medicine in Pittsburgh, explains that substances such as alcohol and opioids hijack the brain’s decision-making abilities. Regaining them can take months. “I have not seen an involuntary hold that would be long enough to help people regain their choice about substances,” she says. “I have a hard time with involuntarily committing someone for that length of time.”
Another complicating factor is that treatment and recovery itself can vary widely. “A lot of times, the perception is that everybody needs residential treatment,” says Michael Langer, who works in behavioral health for the state of Washington. “That’s not true.” Often the best course of treatment, says Langer, is outpatient, or medication-based.
But staffing and funding for treatment facilities of all kinds is in short supply, and getting someone to a short-term treatment facility, with or without their consent, is only a first step on a successful path to recovery. Incentivizing and supporting the individual’s choice to maintain treatment is an equally critical part of the process. That can only happen with a robust and well-funded system that includes many different pathways and interventions.
“I think people imagine there’s this whole massive treatment system,” says Keith Humphreys, who studies addiction and public health at Stanford University. The truth is, he says, most systems across the country – privately and publicly funded – for treatment of addiction are frail and underfunded and can’t accommodate the demand, even from those who are pursuing it voluntarily.
In the United States, a recent report shows that 43% of people willingly seeking treatment for substance use were unable to access it. “Ordering them into treatment is just based on a delusion that there’s somewhere for them to go,” says Humphreys.
Ricky’s law takes shape
Lauren Davis helped to save her friend. In turn, he laid out the path for what would become her life’s work.
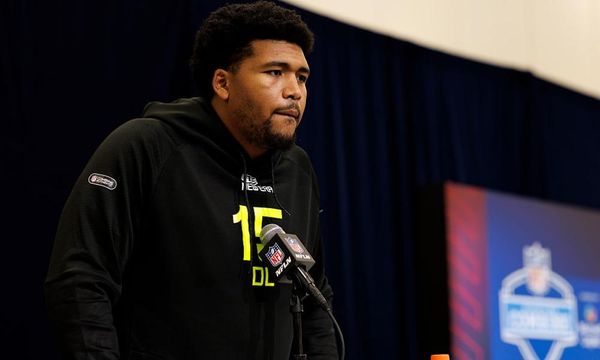
“I started to tell his story to anyone who would listen to me,” says Davis. Some of the people she demanded listen to her were legislators. They helped her introduce a bill for what became Ricky’s law.
After he eventually found his own way into treatment and long-term recovery, Ricky too became an advocate for his bill and Davis’s work. “If this law would have been in place back when I was in active addiction, I believe that my journey would have been cut that much shorter,” he would say in the interview with KNKX. “For a lot of addicts, they want to stop but they can’t. You could have loved ones tell you to stop. You could have all these consequences being behind your actions, and yet you won’t and can’t stop.”
The law amended Washington’s existing rule to allow for short-term, involuntary commitment not only for psychiatric disorders but also for those related to substance use. That meant people “gravely disabled” by addiction – and considered a danger to themselves – could now be committed against their will.
It designated tens of millions of dollars to creating a kind of holding place for detaining people under the law; there are now close to 50 “Ricky’s law” beds in four treatment facilities across the state.
But today, who needs these beds – and how to get them there – is not always clear.
“Someone who comes into the emergency department intoxicated on any substance who is a danger to themselves could be referred right off the bat under Ricky’s law,” says Paul Borghesani, medical director of psychiatric emergency services at Harborview medical center, Seattle’s public hospital. “Practically, that doesn’t happen.”
The reasons are numerous, says Borghesani. Often after 12-36 hours in detox, people who were previously at risk of great harm to themselves “appear much calmer”. Many even say they plan to quit using. This puts the clinicians in a bind, he explains, forcing them to reckon with a philosophical question: is someone a danger to themselves if they claim not to be?
The law is also dependent on a team of mental health professionals called designated crisis responders, employed through state contracts with regional behavioral health agencies and counties. These responders are deployed when someone – often a loved one, community member or medical provider, though it can be anyone – requests an evaluation of an individual in a substance use-related crisis. It’s at the discretion of these crisis responders to decide whether that individual is in enough danger, or endangering others enough, to commit them to a treatment facility – sometimes for just a few days but up to several weeks.
But waits are long for these responders; some advocates for those struggling with substance use disorders report enduring weeks before a designated crisis responder arrives. Sometimes that’s time they don’t have.
Another reason Borghesani says the law isn’t used: hospitals are busy. “Physicians are rightfully very eager to keep people flowing through the emergency departments,” he explains. “So they might look at this as something that would just take a lot of time and not be beneficial.”
Despite these obstacles, Ricky’s law is put to regular use in Washington. According to the Washington health authority, the state has been admitting roughly 700 people annually to substance-use facilities under Ricky’s law.
That number does not reveal how many people have elected to stay in recovery after their forced detention – a fact that makes it hard to say with certainty how effective it has been in galvanizing sustained recovery.
New dilemmas for a new crisis
In 2024, the complex questions raised by Ricky’s law – and what helpful, compassionate addiction policy actually looks like – are more relevant than ever across the country. Recent CDC data shows a stunning national rise in alcohol-related deaths; more than 11% of adults had alcohol use disorder at some point in 2022, according to the National Institutes of Health.
A far more visible catastrophe of addiction is playing out in US cities overwhelmed in recent years by cheap, synthetic fentanyl. In Washington’s King county, home of Seattle, there were more than 1,000 overdose deaths in 2023, a nearly 50% increase from the previous year. Whole blocks are taken over by people buying, using and selling fentanyl. Arguably any one of these people is a grave danger to themselves.
Some outreach workers and medical providers on the frontlines of this problem would like to use the law to help this population, but say it’s not currently possible.
“We get stuck in this place of: what do we do?” says Cyn Kotarski, the medical director with a program called CoLead that helps people with housing and treatment. Kotarski often sees people with abscess wounds, days away from becoming septic. But with long waitlists for designated crisis responders, there’s no way to reach people in these crisis moments. “The option quite literally becomes: they stay outside until they die,” she says.
Frye, the addiction-medicine expert, says the problem is one of more than resources. The US, she says, needs an entirely new orientation to addiction treatment to underpin public policy, one that embraces methods such as harm reduction. “We have to stop being the moral police of people,” says Frye.
Public health addiction crises like the one that Seattle is battling, she argues, would be better addressed by tackling the surrounding problems – housing crises, trauma and mental health issues that give rise to substance use disorders. She imagines coupling this approach with accessible, compassionate therapeutic outpatient settings.
“The best way to help people reduce or stop using substances is to put the patient in the driver’s seat,” she says. “And we as healthcare providers are working towards helping them identify their own reasons to want to come back and quit.” Forced captivity, she argues, doesn’t meet that criterion.
But even Frye acknowledges a utility to saving a person’s life in certain circumstances without their consent. Sometimes her own patients are facing imminent death otherwise. “Transporting someone to the hospital involuntarily, getting that condition assessed, and helping make the hospital stay tolerable for the person – that’s warranted,” she says.
The exact circumstances in which to make this call are hard to define. Maybe impossible.
Inspired by her work creating Ricky’s law, Lauren Davis decided to run for office, and was elected as a state representative in 2018. She has focused her policy efforts on expanding the state’s fragile system of treatment for substance abuse, an endeavor she continues today.
Davis acknowledges Ricky’s law needs course correction to be more useful, and she agrees that even if it’s improved, the law is not enough to adequately address the scope of addiction in places like Seattle.
“Do we just massively scale up Ricky’s law to address the scourge of fentanyl on the streets of Seattle?” she says. “No.”
Instead she’s focusing her current efforts on building a robust system of treatment that addresses comprehensive needs including housing and access to medications like methadone and Suboxone that can be provided over the counter to treat addiction. This effort also includes expanding a recovery navigator program, in which outreach workers build trust with people on the street and help them access resources – willingly.
Still, she firmly believes in the potential and power of Ricky’s law in certain circumstances. She’s seen it work first-hand, saying: “At the end of the day, I believe without a doubt that it has saved lives, that it has changed lives, that it has restored families.”
A devastating turn of events
By late 2020, Ricky had been sober nine years. Then came an episode that would test both Ricky’s relationship with Kelsey and the law created in his name.
Kelsey recalls coming home one day from work and finding his then boyfriend passed out in the stairwell of their condo. Kelsey believes the pandemic triggered the relapse. Ricky had built a network of friends and family in the world of recovery, support that quickly dissolved in social isolation.
“I had heard him talk about what active disease looked like,” says Kelsey. “When it showed up, I was like: ‘Oh my God, what is happening?’”
During that event, according to both Davis and Kelsey, Ricky’s law worked the way it was supposed to. He was put in a temporary, involuntary hold. After a number of days of sobriety, says Davis, her friend re-emerged. “His brain came back online. He was able to make healthy choices,” Davis recounts.
Kelsey says: “He chose our life together.” Kelsey worked to help Ricky gain access to a residential treatment program.
It was more than two years later, after he and Kelsey were married, that relapse came again for Ricky. To Kelsey, it seemed out of the blue. Ricky had gone back to school and had a new job working for an organization supporting recovery for others. “We were really living the dream we always wanted,” he says.
He wonders if his husband was suffering from a kind of existential vertigo. “The only way that I can make sense out of it is that sometimes when things are so good, it’s the fear of losing it,” he says. “That’s what Ricky would talk to me about sometimes.”
This time, in post-pandemic 2023, systems of emergency and crisis support were stressed. Kelsey spent hours on the phone trying to make the legal and healthcare wheels turn in his favor. One night, worried that Ricky was literally going to drink himself to death, he drove his husband to the emergency room. The following day, when there was a staff change, says Kelsey, “the attending physician was going to just release him back out onto the street”.
“I would beg and plead with healthcare staff, police officers. I would say: ‘Ricky’s law is literally named after him,’” says Kelsey.
After Kelsey finally had him committed, Ricky became far less reachable, even after days of forced withdrawal and sobriety. At one point, he fled all the way to Oregon, out of the reach of his own law. Kelsey spent nights with no idea where he was. “I really can’t see anyone living on the side of the street or under an overpass without thinking about Ricky,” he says.
Eventually, Ricky ended up in a residential treatment facility in a Seattle suburb. He went there willingly; Kelsey was expecting to see his husband the next day. Instead, Ricky was found dead.
The cause of Ricky’s death is under investigation. Kelsey is now suing the facility, alleging wrongful death.
Kelsey’s faith in the law named for his husband remains steadfast, as does his belief in the power of recovery. “For anyone dealing with this,” he says, “please know there is hope.”
That optimism has not made his first year as a widower easier. It’s been “hell”, as Kelsey describes it. “I just miss him.”
This story is part of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by the Commonwealth Fund
• In the US, call or text SAMHSA’s National Helpline iat 988. In the UK, Action on Addiction is available on 0300 330 0659. In Australia, the National Alcohol and Other Drug Hotline is at 1800 250 015; families and friends can seek help at Family Drug Support Australia at 1300 368 186
• In the US, you can call or text the National Suicide Prevention Lifeline on 988, chat on 988lifeline.org, or text HOME to 741741 to connect with a crisis counselor. In the UK and Ireland, Samaritans can be contacted on freephone 116 123, or email jo@samaritans.org or jo@samaritans.ie. In Australia, the crisis support service Lifeline is 13 11 14. Other international helplines can be found at befrienders.org