The story so far: For a brief period in October, Mumbai’s air quality matched the stifling haze that covered the national capital, where people complained of burning eyes, choking and troubled breathing. The Air Quality Index (AQI) across different parts of Maharashtra turned from orange (“poor”) to red (“very poor”), crossing the 300 mark. Maharashtra’s health department this week, in its first communique since residents complained of the ‘toxic’ air, introduced a ‘Health Action Plan.’ The civic body will monitor how elevated AQI levels affect pollution-related illnesses across 17 regions. Districts will strengthen surveillance programs to track, how many cardiac, respiratory and other such conditions were reported in a spot with a high AQI.
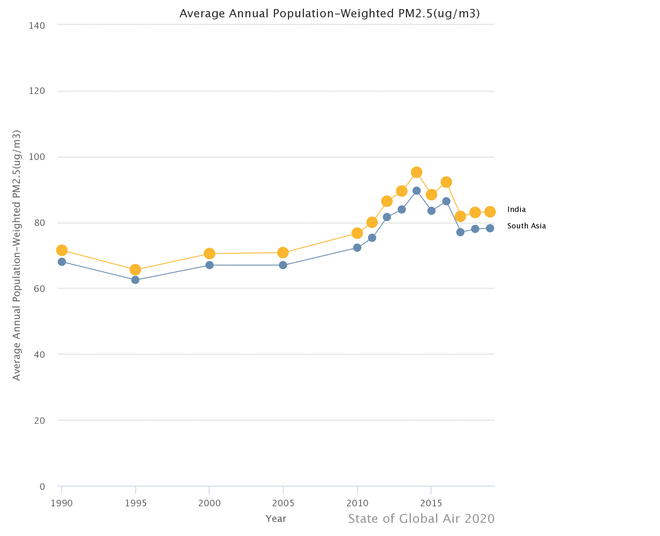
Three of the world’s 10 most polluted cities are in India right now, says Swiss group IQAir. India is also witnessing multiple health alarm bells go off at once — cancer, diabetes and cardiovascular diseases have been called ‘ticking time bombs’, as non-communicable diseases pose a health and economic burden. The 2020 State of Global Air termed air pollution the ‘biggest health risk in India,’ as indoor and outdoor air pollution in 2019 contributed to more than 16.7 lakh deaths linked to stroke, heart attack, diabetes, lung cancer, chronic lung diseases and neonatal diseases.
Weaving health in climate action plans helps plot local patterns of diseases related to air pollution, says Dr. Pallavi Pant, who leads the Health Effects Institute’s Global Health programme; the data can piece together a geographic and epidemiological picture of communities most exposed to bad air, helping to reduce climate inequalities in the long run.
Which illnesses are currently attributed to air pollution?
Research has documented the health risks of particle pollution, a common air pollutant generated by the burning of fossil fuels. Two studies published in international journals last week linked type 2 diabetes incidents with “long-term exposure to ambient PM2.5” in Delhi and Chennai. Air pollution also inflames the risk of obesity, asthma, and cardiovascular disease; people are also vulnerable to dementia and Alzheimer’s disease as bad air impacts cognitive ability. Pollution could trigger lung cancer in non-smokers, too, one study found.
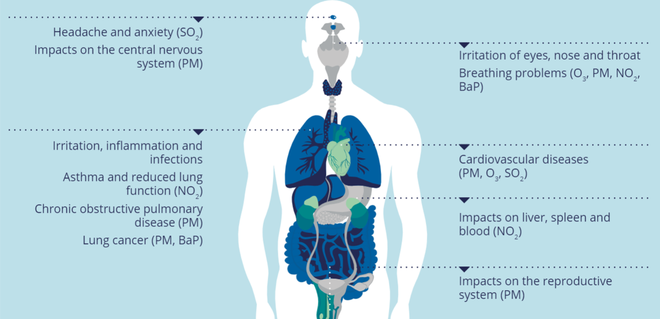
The fine PM2.5 particles (about 30 times smaller than a human hair) travel into the respiratory tract, settle into the lungs and can even enter the bloodstream, triggering immediate and chronic concerns. PM2.5, and its slightly bigger cousin PM10, may both cause irritation in the eye, nose, and throat, along with breathlessness, headaches, coughing and sneezing. In the long run, chronic exposure to PM2.5 could be fatal, as the particulate matter affects every organ in the body and exacerbates underlying conditions. PM 2.5 concentrations originating from fossil fuels in the ambient air caused at least 25 lakh premature deaths in India five years ago, one report found. Children and adolescents are most vulnerable: more than one lakh infants in India died due to air pollution within one month of being born in 2019.
Despite proven risks, “climate action plans are not adequately taking into account the health effects of air pollution,” Dr. Pant says.
All about Particulate Matter
How does Maharashtra propose to monitor illness?
An Indian Express investigation revealed that Brihanmumbai Municipal Corporation (BMC) had failed to issue, and did not have, health advisories for people despite a growing trend of poor air quality. “Mumbai observed 66 poor and very poor air quality days as compared to just 28 in the past three years’ average,” Professor Gufran Baig of theNational Institute of Advanced Studies (IISc, Bengaluru) observed in a report. A Division Bench of the Bombay High Court on November 1 also took suo moto cognizance of Mumbai’s deteriorating air quality. The National Programme on Climate Change and Human Health (NPCCHH) in its 2022 advisory urged States to coordinate with the “concerned departments” to “finalise an action plan to address air pollution-related illnesses”; such an action plan would be activated “during higher AQI levels.”
Under the action plan, Mumbai and 16 other cities will have designated surveillance stations to correlate cases of acute respiratory conditions in emergency wards with monthly data on high AQI levels. “While civic hospitals already collect data, particular focus will be given to respiratory-related numbers,” additional municipal commissioner Dr. Sudhakar Shinde told reporters. AQI data can come from pollution control boards while officials can make use of ICMR-MoHFW documents to make connections, the NPCCHH guidelines note.
District officials are also expected to routinely report and compile data on air pollution-related illness and mortality “for sharing with the National Programme on Climate Change and Human Health program division of NCDC”, to establish trends in the long run. Maharashtra’s plans, and the NPCCHH’s guidelines, require official bodies to prioritise timely and updated air quality forecasting “in a harmonised and standardised way” to make health links. Dr. Pant notes it is equally important that surveillance is carried out year-round, rather than focusing on a few weeks or a few months.
Researchers who looked into the incidence of Type 2 diabetes in two polluted Indian cities, used locally developed high-resolution spatiotemporal models, glycemic markers and incidence of diabetes from a highly polluted region with a high burden of diabetes. Dr. Pant flags that ideally, the team should use pollutant concentrations and not AQI values to study the associations. “It is important to do such analyses carefully and with relevant pollution metrics....and to the extent possible, also take into account other relevant factors — duration of exposure, any pre-existing health conditions, smoking status etc.” In the long run, monitoring health symptoms “must not be done in isolation, but integrated into the larger public health data collection and tracking programs”, adds Dr. Pant.
Officials will also work on identifying hotspots based on AQI levels and where vulnerable populations are concentrated. Some research has highlighted that socioeconomic factors, such as caste, religion and education, in India may present as ‘risk factors’ for exposure to PM2.5. An analysis published in Nature Journal found air pollution was an “emerging axis of inequality” in India. Mumbai’s climate action plan, launched last year with a 2050 deadline to eliminate all carbon emissions, focused on monitoring areas where poor ventilation, use of LPG cooking fuel and occupational hazards thickened polluted air.
The Mumbai Action Plan, in line with the national guidelines, also mentions the need to bolster healthcare services in hotspot areas. This would require technical and personnel infrastructure, training local-level doctors, paramedics and community-level health workers to identify symptoms and create awareness among the local population. People living in severely polluted regions, should have access to plyed masks, medication, healthcare personnel, and emergency ward services. The NPCCHH recommends strengthening surveillance systems, providing timely training to medical officers, analysing data and taking action. Both the national and Maharashtra guidelines, as of now, do not outline the roles and responsibilities of healthcare personnel in such an information-sharing model, or what constitutes an “air-pollution-related illness”.
Dr. Pant avers that public awareness of how pollution impacts health is a key component that continues to lag behind, and “there’s a need for more” initiatives at the State and district level.
How can this data be used?
In the long run, well-maintained surveillance records serve two purposes: estimating and preparing for poor air quality events, while also mapping health benefits in case air quality improvements are made, Dr. Pant points out. In an ideal scenario, Dr. Pant says the team should track both air quality and health data together, and “identify a short list of key health outcomes to track over time.” For instance, short-term exposure to bad air can result in respiratory infections like pneumonia, and officials can track hospitalisation rates and OPD visits at periods when particulate matter concentration is high. Data can surveil both frequency as well as magnitude, capturing how much infections rose thus piecing together “the magnitude of health impacts.”
Such correlations exist anecdotally right now. Dr. Alpa Dalal of Jupiter Hospital told Scroll last year of a “noticeable” rise in respiratory illnesses following an increase in air pollution; other doctors confirmed the trend but this observation has so far lacked precise numbers and characteristics. Health departments at present do not require mandatory reporting of conditions like bronchitis or asthma during pollution events. Dr. Lancelot Pinto, an epidemiologist and pulmonologist, said the data can eventually become a “transparent repository and can help citizens to better appreciate the harms associated with air pollution and see overall trends”. The medical community can also partake in establishing standard reporting procedures and a consensus on defining such a disease burden. “We mobilised such data collection during Covid, do it regularly for TB… it would serve both citizens and policymakers to do the same for air pollution-related illnesses,” he told The Indian Express.
Better data and evidence can unearth local patterns of diseases; children, pregnant women, the elderly, people with pre-existing cardiovascular and respiratory conditions, and those living in low-income socio-economic conditions are identified as “vulnerable groups” under the NPCCHH. Researchers found the greatest increase in PM2.5 concentrations was in less urbanized districts with a high percentage of SCs, women, children, persons with disabilities, and households without toilets. Linking health diseases back to pollution can subsequently inform health advisories to protect vulnerable groups. Take West Delhi’s Mundka region, where AQI crossed the hazardous 400 mark this week. Data from local mohalla clinics and hospitals could potentially “help develop targeted programs aimed at reducing exposures” among disadvantaged communities, says Dr. Pant. For instance, policymakers could install indoor air purifiers in community settings for individual and environmental well-being. Moreover, if Spot X registers increased cold and cough cases, interchanging data between pollution control bodies and district health officials could ensure local dispensaries are equipped with the right medicines and healthcare support.
Bad air imperils not only the environment but health infrastructures too, and policymakers will have to train their attention to public health challenges as well, says Dr. Pant. Air pollution and illnesses both add to India’s expenditures: research shows the rising trend of non-communicable diseases would increase health-related expenditures, while estimates show economic losses due to pollution amounted to 1.36% of India’s GDP in 2019. “As air quality management strategies continue to expand, a focus on health can also help us look at how the interventions being introduced can improve public health,” Dr. Pant notes.
Writing in The Wire, climate researchers previously expressed dismay at India’s sluggish progress towards developing a climate change-resilient healthcare system, the absence of which widens health inequalities. Establishing surveillance systems like Maharashtra’s Health Action Plans is a step in that direction. This, along with strengthening healthcare infrastructure, promoting research on climate-health linkages, and building healthcare personnel’s capacity can help India adapt and mitigate a health crisis within a climate crisis.
Such interventions, however, “can only go so far”, adds Dr. Pant. “The largest improvements will come from reducing air pollution emissions at source.”
Health advice for people with pre-existing conditions
- The Air Quality Index (AQI) across different parts of Maharashtra turned from orange (“poor”) to red (“very poor”), crossing the 300 mark.
- Research has documented the health risks of particle pollution, a common air pollutant.
- The Mumbai Action Plan, in line with the national guidelines, also mentions the need to bolster healthcare services in hotspot areas.







