More than 16,000 hospitalisations a year for chronic conditions in the Hunter health network are potentially preventable, national health data shows.
This amounted to 80,815 days in hospital.
Chronic conditions include asthma, congestive cardiac failure, diabetes complications, chronic obstructive pulmonary disease (COPD) and hypertension.
The conditions are considered preventable as they could have been controlled through "primary and community care interventions" from a GP or nurse.
The Australian Institute of Health and Welfare data also documents preventable acute conditions.
In the Hunter network, which includes New England and Central Coast, 15,284 hospitalisations for acute conditions were preventable.
This amounted to 60,461 days in hospital.
Acute conditions usually come on suddenly, and may not be preventable, but hospitalisation could have been avoided if "timely and adequate care had been received".
Acute conditions include pneumonia, urinary tract infections, bleeding ulcer, cellulitis, ear, nose and throat infections and dental problems.
The data, which applies to the 2021-22 financial year, included vaccine-preventable hospitalisations.
In the Hunter network, there were 1557 of these cases which required 9849 days in hospital.
This included 1132 hospitalisations for pneumonia and influenza cases that could have been prevented with vaccination.
An AIHW report said primary and community health care "can be an opportunity for early intervention".
This could help reduce the risk of a person "developing a disease, their symptoms worsening or complications developing to the point that they need a hospitalisation".
The Hunter network's rate of hospitalisations for chronic and acute conditions per 100,000 people was 890 and 1039 respectively.
This was higher than Central and Eastern Sydney (695 and 903), Northern Sydney (564 and 887), Western Sydney (731 and 817) and South Western Sydney (744 and 861).
Western NSW (984 and 1160) had a worse rate than the Hunter network, along with North Coast (926 and 1324).
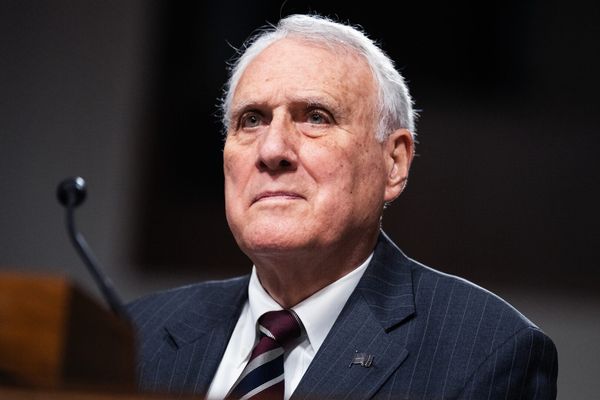
Max Mollenkopf, of Whitebridge Medical Centre, said "there are more older people living with more disease".
"More and more of that is being managed in the community [such as GPs]," Dr Mollenkopf said.
The Royal Australian College of General Practitioners (RACGP) Health of the Nation 2023 report said GPs received less than 7 per cent of overall health funding.
"That is pretty inadequate when you look at the burden of chronic disease we look after," Dr Mollenkopf said.
He said this was why costs were "so high" for people to see a doctor.
GP fees in Newcastle for a standard consultation have risen to more than $100, with patients receiving a Medicare rebate of $42.85.
"More and more GPs are just reflecting the cost of care [in their fees]," he said.
This made it harder for patients with chronic disease, for example, to manage their care at GP clinics "because they can't afford it".
The British government was diverting billions of pounds from hospitals to GPs to "fix the front door to the NHS", the Guardian reported last month.
Dr Mollenkopf said the move was aimed at "reflecting the fact that more complexity is being managed in general practice".
"There's an old analogy - why are you putting more ambulances at the bottom of the cliff when you could be putting GPs up the top of it?
"For every dollar you spend in general practice, you can see a total health saving that is significant and valid.
"This is the type of structural reform that a government would need to take. It takes a bit more bravery than just funding a healthy heart check as a cheap band aid solution."
University of Newcastle nutrition professor Clare Collins told the Newcastle Herald in March that it was time for the federal government to crack down on junk food marketing to kids.
The government released a feasibility study in February on options to limit this type of marketing.
The World Health Organisation said in June that one third of adults worldwide, about 1.8 billion people, "did not meet the recommended levels of physical activity in 2022".
"Physical inactivity is a silent threat to global health, contributing significantly to the burden of chronic diseases," said Rudiger Krech, the WHO's director of health promotion.