
There has to come a point where doctors decide, I can’t do my job any more – and then the situation will spiral out of control. I would use the term ‘crisis’: so many parts of the NHS are under such enormous pressure that they are unable to provide the personal care that patients need, unable to provide effective care, and increasingly unable to even provide safe care.
In a speech to mark the 70th anniversary of the founding of the Royal College of General Practitioners reported in the Observer, its outgoing president Martin Marshall was blunt about the state of his profession. His fears for GPs’ futures were echoed across the media throughout the winter of 2022, amid warnings of a “tsunami of demand” from the public. In January, a member of the GP Survival network wrote that the pressures had got too much:
I’m only 58 but I’m retiring in March. I can’t cope any more with the stress and overtime being a GP involves – doing the job of two people while GPs are criticised regularly by the right-wing media … I am too overloaded and don’t really see the point when my patients are being harmed by delays across the NHS and care services.
In March, the Health Foundation – one of the UK’s most influential independent health bodies – published a survey of nearly 10,000 GPs in ten countries around the world. Some 71% of UK GPs said their job was “extremely” or “very stressful” – the highest of the ten countries surveyed, alongside Germany. The report concluded:
Results from this survey and others show alarming numbers of GPs looking to leave the profession, reduce their hours, or stop seeing patients in the near future … The experience of GPs in the UK should ring alarm bells for government.
Over the past decade, one in five practices in England and Wales have closed. The multiple challenges facing GPs show no sign of receding, despite the reduced threat posed by COVID. In May 2023, Anita Raja, a West Midlands GP, told Sky News:
GPs are at breaking point. We’re immensely understaffed. Partners are leaving their partnerships, practices are closing down. If it goes on the way it is, we will have no primary care any more.
For many UK GPs, the seemingly endless demands on their time and “overwhelming” number of patient contacts are key components of work-related stress. A significant amount of a GP’s day is now spent on clinically-demanding background work, such as making sure that all test results are understood in the context of each patient, and that actions recommended by hospital specialists are appropriately put in place.
“It’s the boiling frog analogy,” Bob Hodges, a Gloucester GP, told the Observer. “The water’s not been comfortable for a decade, but it’s now very noticeably warmer. It will soon reach a threshold where there is a collapse.” In the same article, Rowena Christmas, a GP in Monmouthshire, offered this chilling warning:
I do sometimes feel we are in [the] dark last days of this way of doing things, and it really makes me feel sick to say that … If we lose general practice, we lose the NHS as we know it, with all the awful health inequalities that will follow.
The link between stress and GP shortages
Many GPs say they have long felt undervalued by the general public, the media and the government – with negative media portrayals of remote GP consultations during the pandemic only adding to these criticisms. Many believe they are being blamed for the fallout from more than a decade of underinvestment in primary healthcare.
The increasing levels of work-related stress and low morale is having a damaging effect on recruitment and retention of GPs across the UK. Dissatisfaction with working in the UK is also a factor in some doctors’ decisions to take their qualifications overseas.
The Royal College of GPs has predicted a “mass exodus” of GPs and trainees in the UK over the next few years. Its 2022 survey of 1,262 GP and trainee respondents in England found that 42% were “likely” to quit the profession within the next five years. One in ten said they expected to leave within a year.
Analysis of the latest workforce data confirms a continuing drop in England’s number of GPs – the equivalent of 2,133 fewer fully qualified, full-time GPs than in September 2015. At the same time, GPs’ working hours have increased and the number of appointments delivered in England continues to exceed previous monthly records.

To mark the 75th anniversary of the launch of the NHS, we’ve commissioned a series of articles addressing the biggest challenges the service now faces. We want to understand not only what needs to change, but the knock-on effects on other parts of this extraordinarily complex health system.
Yet difficulties in accessing NHS GPs – including the infamous “8am scramble” for on-the-day appointments – remain of major public concern. In 2023, a widely circulated joke suggested trying to buy a ticket for comedian Peter Kay’s latest tour was as hard as getting a GP appointment.
One policy response has been to bring in many non-GP practitioners to work alongside GPs in their surgeries. However, our May 2022 study found that the need for GPs to provide ongoing supervision and support for these staff, some of whom have little or no experience of working in general practice, has created a new and, for many GPs, unexpected workload.
The new NHS Long Term Workforce Plan for England, announced today, promises a 50% increase in the number of GP training places to 6,000 by 2031, with GP trainees due to spend their entire training in general practice. The new plan has been described by Amanda Pritchard, chief-executive of NHS England, as a “once in a generation opportunity to put staffing on a sustainable footing”. Its effectiveness in resolving the crisis in general practice can, in part, be assessed against achieving increases in the number of GPs that previous government pledges have failed to deliver.
In May, health minister Neil O'Brien told the BBC that “we’ve got 2,000 more doctors working in general practice than we did in 2019 before the pandemic”. But this figure included trainee GPs – and according to an analysis by the Institute for Government, the qualified GP workforce has gained little from this increase because recently trained GPs are now leaving UK general practice at an unprecedented level. In its March 2023 report, the Health Foundation concluded that, in England:
Despite repeated government pledges to increase the number of GPs … shortages are estimated at 4,200 and could grow to 8,800 by 2031 – around one in four projected GP posts.
GPs as ‘conductors of the orchestra’
You have so little time to develop relationships with people – to get to know them as you could do in the past. That impacts on clinical decision-making as well – as every patient is new. So, you cannot take any risks. (Reflections of a GP and teaching facilitator)
The GP practice as a continuously available social safety net – a place where doctors have a sense of who you are over a long period – increasingly feels like a thing of the past. In part, this may be a product of changing expectations in this “digital first” age of convenience. Relationship-based care by GPs with whom you can share the story of your life and that of your loved ones, even tangentially, may not be what young and fit people assume they need any more.

In fact, the average age of the UK population is rising, and with it the number of people requiring ongoing care for (often multiple) long-term conditions and increasingly complex care pathways. Yet the work of GPs has become increasingly shaped by requirements to follow standardised care pathways and achieve specific performance targets. This means the GP’s traditional role as “conductor” of the healthcare orchestra – as opposed to merely a “gatekeeper” – is increasingly difficult to carry out.
An example of the everyday emergence of nuance and complexity in relationship-based care is illustrated in the following anonymised account of a patient seen by one of this article’s authors (Harm), when he worked as a practising GP:
Mr Wei, 59 years old and originally from Singapore, visits the surgery to discuss a cough. He is also hoarse. It is summer, and these problems have been going on for six weeks.
Mr Wei has lived in the UK for more than 30 years. For most of his life, he has smoked more than 30 cigarettes a day. He lives alone and works as a chef in a Chinese restaurant. He has to work very hard under less-than-optimal circumstances, and appears socially marginalised.
To the GP, it is not immediately clear what the purpose of Mr Wei’s visit is. He appears reluctant to discuss his symptoms, and says he isn’t worried about his health at all. But medically, the patient qualifies for an urgent ear, nose and throat referral to detect any early cancer, and the GP also suggests a chest X-ray. No abnormalities are found during these subsequent examinations.
A month later, Mr Wei returns to the GP surgery to discuss what next steps could be taken for his cough. But support to quit smoking is not an option, he says, as it helps him with his stress.
The GP explains there are no drugs that really work for cough. Mr Wei says he understands, and that Chinese medicine could not help him either. He says there are many complicated issues in his life, but that he cannot discuss them.
Mr Wei keeps coming back every three weeks over the next several months, usually with a new symptom of potentially significant medical concern, such as unexplained weight loss – another symptom that warrants an urgent referral.
Over the visits, a measure of mutual trust develops between GP and patient. Mr Wei is not looking for referrals, it transpires, but just wants the GP to be aware of each new symptom and take responsibility for them. In his previous clinical practice in the Netherlands, the GP (relying on clinical experience) would have assumed medical responsibility for deciding not to refer the patient in this situation.
However, in the UK, these many encounters play not only into a professional sense of guilt for spending a lot of time with this patient, but also of feeling “policed” – as if under obligation to respond in ways that were neither required nor wanted by the patient. The GP realises that the pervasive NHS “utility thinking”, with its focus on doing rather than listening, has entered his clinical awareness – and indeed, has overtaken it. His conclusion? It is time to stop practising as a GP.
Today’s GPs face an uphill struggle. Under severe time pressure, they are often unable to integrate the personal (the patient’s life story and relationship with the GP) with the medical (a hi-tech, interventionist approach that demands increasing levels of specialisation). This is how discontinuation and fragmentation win, and how the core value of general practice – connectedness through continuity – has been diminished or lost.
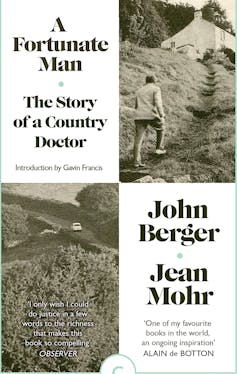
More than half a century on from John Berger’s influential 1967 work A Fortunate Man, about a country doctor who trained as a surgeon but became a good GP by listening to his patients, we increasingly regard quality of GP care as something quite different. These days, it is contained in data such as: how long patients wait for an appointment, how close their blood pressure or sugar levels are to recommended levels, or how optimised is their medication regimen.
For many GPs, having fewer opportunities to engage directly with patients has led to a loss of professional satisfaction. It is perhaps a symptom of a loss of trust in medical professionals that their performance has become so heavily measured by adherence to impersonalised rules, guidelines and protocols. This, of course, modifies definitions of what constitutes “good” general practice, and, in the view of many GPs, makes it more difficult for capable and committed professionals to deliver the care that patients want and need.
Once lost, trust and confidence take time to rebuild – or, as the Dutch saying goes, “trust comes on foot and leaves on horseback”. When so much of their effort is being diverted to satisfy intrusive monitoring, many GPs no longer consider themselves fortunate men or women.
The impact on patients
Patients are also suffering the ill-effects of the GP workforce crisis. The national GP patient survey has shown an unprecedented fall in their overall experience of general practice, with patients living in the most deprived areas reporting the least-positive experiences.
GPs themselves often express concern that their workforce pressures and heavy workloads are increasing the risk to patient safety – and, in the event of medical litigation, to their own professional accreditation. In the Royal College of GPs’ survey, 65% of respondents said that patient safety is being compromised due to appointments being too short. In May 2023, the college’s incoming chair, Kamila Hawthorne, told the Guardian:
Patients getting sicker while they are on the waiting list is something GPs see and worry about … It could be someone awaiting a hip or knee replacement – often the waiting times for orthopaedics can be a year or two, so you know it’s going to take ages. They’ll tell you their toilet is upstairs and that to get up there, they’re having to crawl … Or that the pain is coming to the point where they can’t sleep at night. That’s the kind of thing we hear.
GPs regularly deal with patients frustrated about long-delayed hospital appointments and procedures. Such issues were exacerbated by the pandemic, which also triggered an abrupt change in the way many GP consultations were carried out.

Early in 2020, a rapid switch from in-person to remote consultations was mandated by the UK government as part of efforts to reduce the spread of COVID-19. Initially, this was widely seen as a positive innovation that contributed to both patient and staff safety. However, by 2021, concerns were being raised in the media about the quality and safety of this “remote consulting” system, as well as the digital inequalities it highlighted among the elderly and most vulnerable.
Numerous analyses of patients’ access to GP appointments continue to emerge. While national data indicates a significant increase in the number of appointments (both in-person and remote) being provided, reports suggest that as many as a quarter of accident & emergency patients may have gone to hospital because of the length of GP waiting times, and that growing numbers of people are turning to private GP services “amid frustration at the delays getting an appointment with an NHS family doctor”. According to David Hare, chief-executive of the Independent Healthcare Providers Network: “Private GP services are one of the big growth areas of a burgeoning private healthcare sector.”
In January, GP Jenna Fowler told the Guardian:
When I see or speak to a patient for the first time, I often spend the first few minutes explaining the situation or apologising for delays. Unfortunately, patient dissatisfaction has led to increased reports of abuse towards healthcare staff, which is upsetting and demoralising at a time when we are working so hard to do the best we can for our patients.
Following the death of Gail Milligan, a Surrey GP who took her own life in July 2022, her husband Chris spoke to the healthcare professionals website GPonline about the need to protect GPs from the extraordinary pressures now being placed on them – including from the public:
I would really want public opinion to start changing. I understand people being frustrated because they can’t get a doctor’s appointment, but they need to know the real story of what’s going on behind the scenes, and how hard these people are working – that doctors are dying to offer services they know aren’t up to scratch any more.
A whole other level of stress
Being a GP now is just awful. You are hung out to dry. The risk is all yours … By introducing privatisation at scale, [the chancellor] Jeremy Hunt and his friends are bringing down what is to me a very valuable resource. American companies are now taking over chains of practices. (Reflection of a current GP)
General practices operate under a nationally-agreed contract between the Department of Health and the British Medical Association (BMA) to deliver comprehensive healthcare to a registered set of patients (with some variations in Scotland, Wales and Northern Ireland). The contract holders – typically, GP partners – bear responsibility for their practice’s business operations, including the expenses incurred in the employment of staff (clinical, managerial and administrative) and provision of premises.
This partnership model – the main legal structure for general practice since the NHS was established in 1948 – has proved resilient in the face of policy changes, and has successfully adapted in response to changing health priorities. But for the GP partners who make up just over half of all UK GP roles (compared with more than 40% who are in non-partner, employed positions), the relative freedom and opportunities of the partnership model come with a large amount of additional work – and the potential for stress and worry.
Most GP partners operating under this small business model feel far removed from national-level decision-making processes. Yet the business risks, contractual responsibilities and financial pressures they personally hold have increased significantly in recent decades. As Bob Hodges, a Gloucester GP, told the Observer:
There is always the threat in small partnerships of being the last man standing; if you are in a partnership of two and your partner resigns, then you have all the financial liability of an asset you are not allowed to sell.
Policies introduced by both Conservative and Labour governments have complicated the GP partnership model by focusing on solving particular problems – for example, prioritising speed of access over continuity of care, leading to patchwork contractual arrangements and add-on payments. Meanwhile they have failed to resolve key issues such as the shortage of available GP appointments in areas of greater social deprivation and poorer health.
The increased requirement for performance monitoring and target-driven performance incentives that accompanied the 2004 version of the national GP contract have also created much additional work for GP partners, making the prospect of running a sustainable general practice ever-more challenging.
Resources and facilities in many GP surgeries are also sub-standard. More than a third of GP respondents to the Royal College of GPs survey said their practice premises are not fit for purpose (38%), and that IT for booking systems are not good enough (34%).
Yet much of this slips under the radar – until, periodically, practices “fail” or hand back a contract when they can’t recruit sufficient staff to deliver a safe service.
The precarious financial status of general practice was highlighted during a recent House of Lords debate. Responding to concerns that GP practices were at risk of being bought out by US companies, Nick Markham, a government health minister, admitted that “it is not a massively profitable area at the moment”.
Meanwhile, data on GP incomes contradicts some media suggestions of “fat cat” salaries. When reduced hours and inflation are taken into account, GP income reduced by 10% for partner GPs and by 7% for salaried GPs between 2008 and 2017. In 2022, it was revealed that, despite the Department of Health’s recommendation of a pay rise for general practice staff, there would be no adjustment to practice funding to reflect this.
What can be done to address the GP crisis?
The first step to solving a problem is to acknowledge it, and we believe that general practice is in crisis. It is clear from the latest GP patient survey results that, despite the best efforts of GPs, the elastic has snapped after many years of pressure.
This Future of General Practice report, compiled by the cross-party Health and Social Care Committee after taking evidence from many sources, went on to conclude that:
Patients are facing unacceptably poor access to, and experiences of, general practice. Patient safety is at risk from these unsustainable pressures … [But] given their reluctance to acknowledge the crisis in general practice, we are not convinced that the government or NHS England are prepared to address the problems in the service with sufficient urgency.
As academics working closely with GPs and listening to daily accounts of life on the “frontline”, we do not believe there is a magic solution to the challenges they face – but our research, observations and experience point to three key areas for action.
1. Make general practice a more attractive career
Job satisfaction for GPs is closely linked to having the time and space to achieve the professional standards they aspire to – placing greater value on responding to the real-life needs of patients such as Mr Wei, than on achievement of incentivised targets that may be poorly aligned with patients’ needs.
While GPs are already distributing elements of their work to other trained staff, many continue to feel overwhelmed by administrative work of low clinical value, and by the volume of work now being transferred to them from other health providers. For example, recommendations designed to reduce requests for GPs to take responsibility for checking patient investigations (rather than the hospital team who originated them) have so far had limited effect.
2. Emphasise the importance of the ‘expert generalist’ role
One of the most prominent policies to address the primary healthcare workforce crisis in England in recent years has been the recruitment of different types of non-GP practitioner, such as pharmacists, paramedics and physician associates. The idea is that, as less complex casework is diverted away to these other practitioners, GPs are able to spend more time dealing with complex cases.
However, our research shows that GPs’ overall workload and job satisfaction levels have not improved through implementation of this policy, which also risks reducing the continuity of a patient’s care. It is a sticking plaster that cannot seamlessly fill the gaps arising from the GP crisis.
The newly-announced NHS Long Term Workforce Plan promises ambitious ideas for different approaches to training clinical staff, as well as actions to improve staff retention across the NHS workforce in England. Sustainable work schedules, including adequate time for GPs to provide expert clinical support for colleagues, should be an integral part of this plan.
It is important that all practitioners entering general practice – whatever their specialism – receive training and experience to prepare them for the immense breadth of general practice casework. The importance of the “expert generalist” role must not be lost in any restructuring of the primary care workforce.
3. Give GPs more choice in how to run their practice
In recent years, there has been a gradual reduction in the proportion of GPs who work as GP partners. Pointing to this decline, some health commentators suggest this contractual model is no longer the best way to organise general practice. The threatened closure of GP practices has, on occasion, seen community trusts (or other bodies) take over these practices, offering GPs an option to work under different contractual conditions.
However, the Royal College of GPs remains positive about the “exceptional” added value brought to general practice by GP partners who, often at personal cost, are committed to supporting their staff and serving their communities. The cost-effectiveness of this contractual model was confirmed by an independent review of GP partnerships in 2019.
Ultimately, whichever model (or combination of models) is adopted, turning the tide for general practice demands a clearer understanding of the GP’s role and how to support it. This includes motivating and empowering the general public towards healthier lifestyles – and, if capacity and capability of the GP workforce can be increased, rebuilding public confidence in this frontline of healthcare. The situation is critical.

For you: more from our Insights series:
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter.
Sharon Spooner has received funding across several projects from the National Institute for Health Research (NIHR) and The School for Primary Care Research through the University of Manchester. The views expressed here are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care or the Health Education England.
Harm van Marwijk was supported by the National Institute for Health Research (NIHR) Applied Research Collaboration Kent, Surrey, Sussex. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Imelda Mcdermott receives funding from the National Institute for Health Research (NIHR) and Health Education England (HEE) through the University of Manchester. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care or the Health Education England.
This article was originally published on The Conversation. Read the original article.







