
You know E. Coli as the illness you can get from unpasteurized milk or contaminated romaine lettuce. But only a few strains of the bacteria make you sick. Most are harmless or helpful members of your body’s lively internal ecosystem, the microbiome.
There are about as many microbes in and on our body as there are cells, and they do things that our cells can’t, like digest fiber and generate vitamins. Altogether, these organisms comprise around 46 million genes that build proteins — thousands of times more than our own DNA’s 20,000 protein-coding genes.
Scientists have long tried to hack into this genetic diversity to prevent or treat diseases that affect our bodies and brains. Now, they may have broken down a key barrier to targeting disease using mice — the innovation may eventually be applied to humans to develop a long-lasting treatment for complex conditions like diabetes.
What’s new — In a study published Thursday, August 4, in the journal Cell, researchers tweaked the genome of a strain of E. Coli taken from mouse poop, coaxing it to produce an important enzyme that could help protect the mouse against diabetes. Then, they put the edited bacteria back into mice. It remained in their guts and continued producing the beneficial enzyme for months, lowering the mice’s blood sugar and insulin levels.

These results find an “elegant, practical way” around a major roadblock that has stood in the way of this type of treatment, called live bacterial therapeutics, says microbiome expert Nathan Crook — namely, getting the engineered bacteria to thrive once it returned to the mice’s gut. Crook is an assistant professor at North Carolina State University and was not involved in the new research.
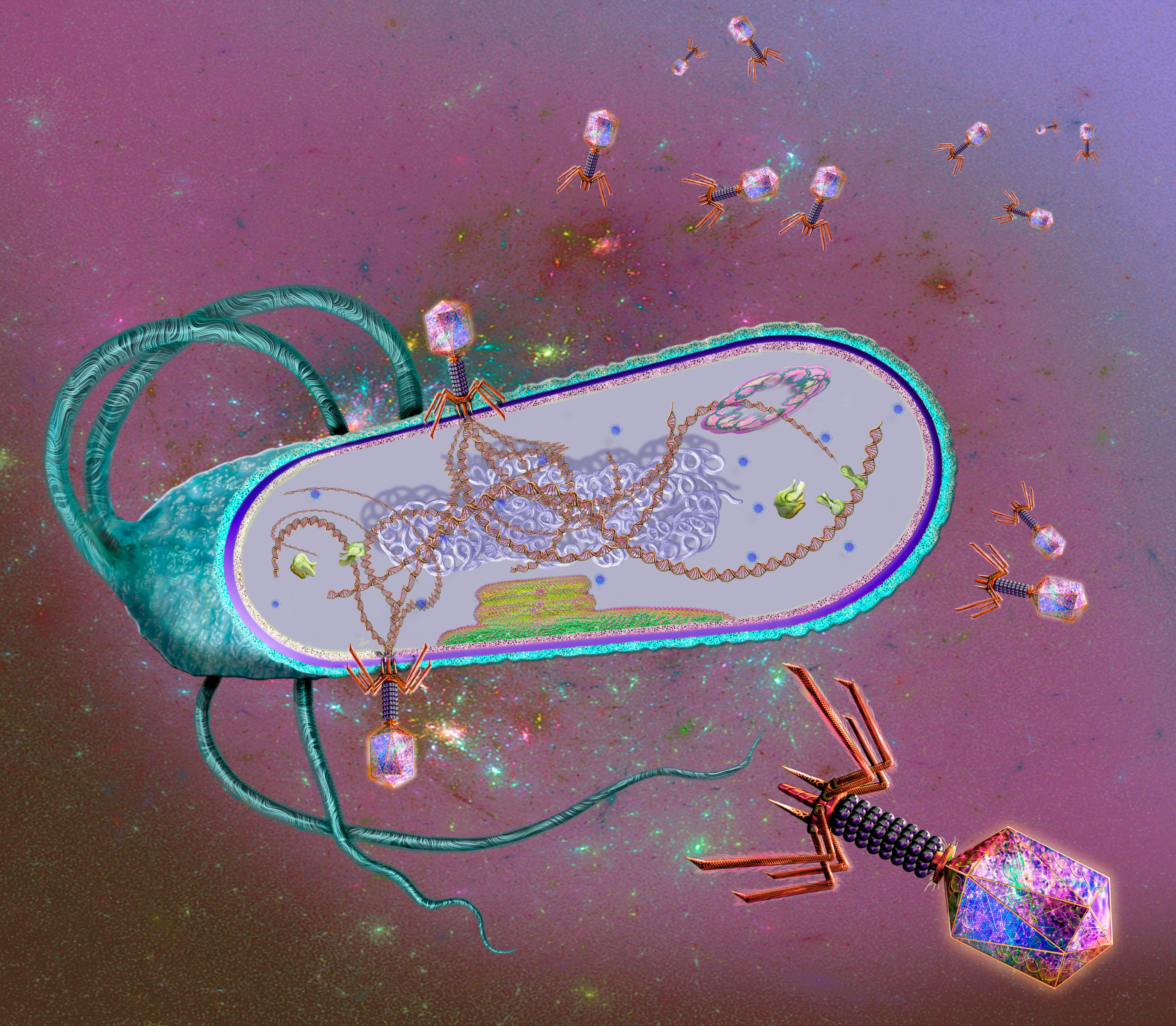
To elaborate a little on the issue: Scientists could genetically engineer bacteria to perform all sorts of biological tricks in the lab, but they didn’t make it once they went back into the gut. That’s because the gut is a haven for its microbes but a hostile place for new organisms trying to make a go of it. So these researchers decided to take a Trojan Horse approach with the mouse’s native E. Coli.
“The hope is that one day, we can engineer a person's microbiome to fight disease for them.”
Unlike lab-grown strains of the bacteria, this undomesticated E. Coli could hold its own in the mice’s gut once it was genetically altered and fed back to the mice.
“It’s very well adapted to go back and become part of the community,” says Amir Zarrinpar, one of the study’s co-authors. He is a gastroenterologist researching the gut microbiome at the University of California, San Diego.
The engineered E. Coli continued to produce an enzyme called bile salt hydrolase and altered some key features of the mouse’s metabolism for the rest of its life following the treatment.
Why it matters — For now, these results are just in mice, and we can’t assume that the findings will translate elegantly to humans — but they do give scientists a novel protocol to try and replicate the effect in human guts. If scientists can use our bacteria to alter our metabolic health for the better, then it could help prevent disease.
“The hope is that one day, once we have a better idea of how to control the functions of the bacteria, that we can engineer a person's microbiome to fight disease for them,” Zarrinpar says.
Zarrinpar and his colleagues hope to develop long-lasting treatments that don’t require daily doses of medication. One day, they may engineer bacteria that fundamentally transform the body to treat conditions affected by the microbiome and metabolism — diabetes, inflammatory bowel disorder, and irritable bowel syndrome, to name a few. Zarrinpar is also the co-founder of a biotech company called Endure Biotherapeutics, which has a patent pending on the techniques described in the new study to take this idea forward.
In the study, the authors do take the first step to this end: They isolated and genetically edited a comparable strain of E. Coli from human stool. We don’t yet know how the bacteria would fare in the human gut, how they would affect our physiology, or how safe and effective the treatment is in humans. To answer these questions requires a human study and trials.
Still, Samuel Forster, who researches the gut microbiome at the Hudson Institute of Medical Research in Australia, says that “the research represents an important step forward in the development of genetically engineered live biotherapeutics.” Forster was not involved in the study.
Engineering the future — One issue with this potential treatment is that some microbiologists aren’t even sure scientists should be trying to find permanent or even semi-permanent hacks for the gut microbiome.
Suppose an engineered E. Coli sticks around in a person’s gut. In that case, it may pick up undesirable genes from its neighbors in a way scientists can’t yet predict, according to Bruno Pot, a microbiologist. He researches live biotherapeutics at Vrije Universiteit Brussel in Belgium. He was not involved in the study.
Rather, Pot argues it would be better to find ways to achieve the same effects without expecting the engineered bacteria to permanently reside in the body. If something unexpected happens, pausing treatment would be much easier than trying to reverse-engineer what was supposed to be a long-term fix.

“The main question is how to remove genetically modified bacteria once it’s no longer needed or shows harmful effects,” says Natalia Shulzhenko, an immunology and microbiology researcher at Oregon State University. It would be better to have “full control of its fate,” she says. For their part, the researchers behind the paper agree that there needs to be a degree of control before their work makes it to humans in a clinic.
“I think before this goes primetime to humans, we just really need to have good ways to control the therapy as well as we can,” says Zarrinpar.
What’s next — There’s a lot of work that needs to happen before this technique is ready for human testing. Currently, Zarrinpar’s lab is working to isolate and genetically modify native human E. Coli more efficiently.
They are considering testing the technique in pigs, as well, since their gastrointestinal tract is more similar to ours, which may offer a better translational model to develop a protocol for use in humans.
To hone this treatment for humans, researchers may begin with metabolic issues with a clear cause and effect, like phenylketonuria, Zarrinpar says. People with this rare condition don’t produce the enzymes that break down the amino acid phenylalanine, which can build up as a result and cause brain damage and seizures.
This small group of people, like so many with rare diseases, also have very few treatment options, but an opportunity may lie with bacteria that have been engineered to produce the missing enzyme.
“These microbes that are essentially part of us — they’re portable toolkits already — will have this engineered addition of a tool where they are helping us fight disease,” Zarrinpar says.







