The proportion of GPs in England working full-time at local surgeries has fallen to the lowest level since current records began five years ago, figures show.
Nearly a quarter (23%) of qualified permanent GPs worked at least 37.5 hours a week in June 2022, down from almost a third (32%) in June 2017.
The number of family doctors working full-time hours or more has dropped in the same period from 10,740 to 8,207.
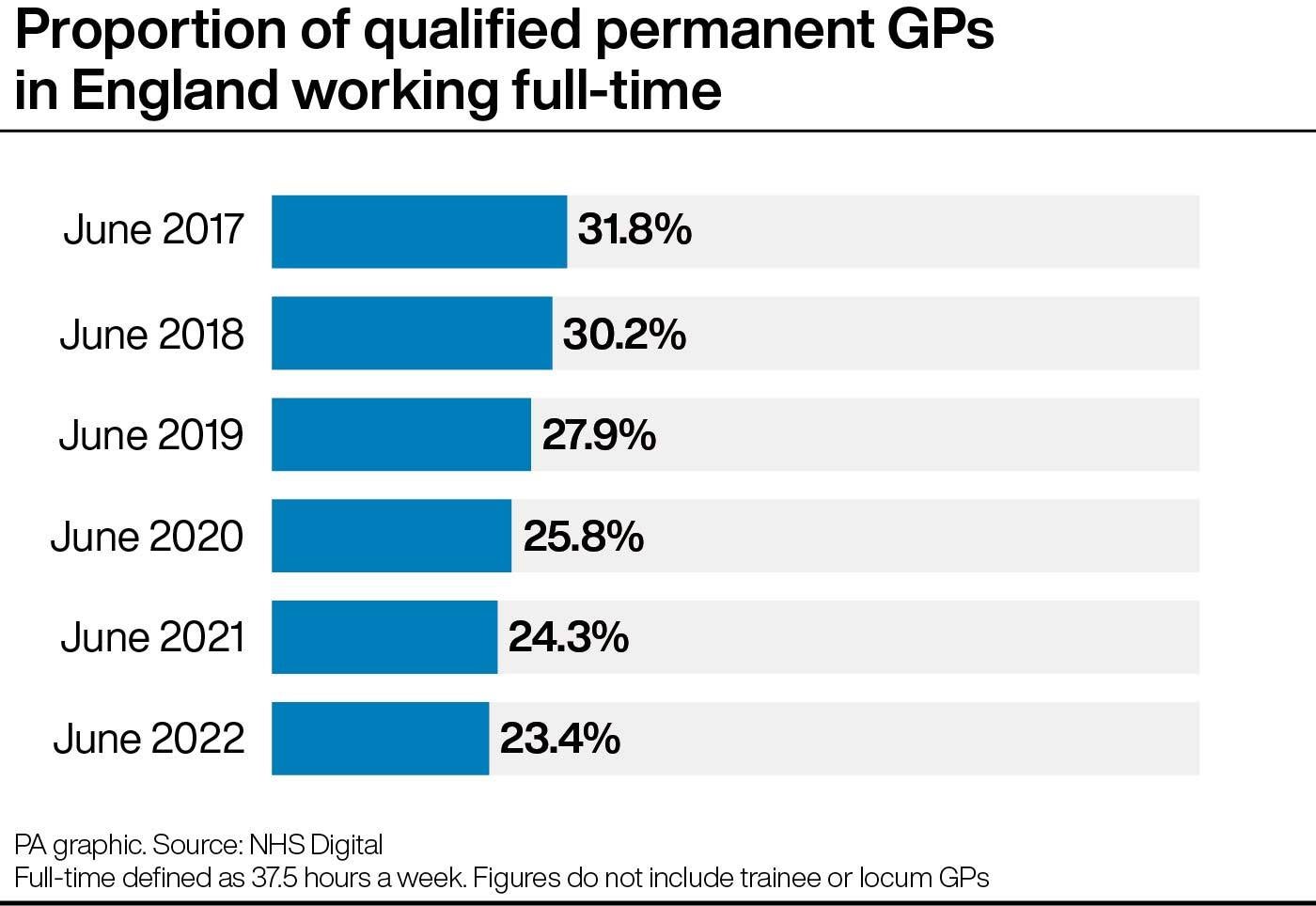
At the same time, the proportion of GPs working between 15 and 37.5 hours a week has climbed from around six in 10 (62%) to seven in 10 (69%).
Beccy Baird, senior policy fellow at the King’s Fund think tank, said that while the data may show fewer GPs contracted to do full-time hours, many were still working very long days.
She told the PA news agency: “They might be contracted to work six sessions a week, which is three days.
“But those could be 12-hour days, so on paper it’s 24 hours a week but actually in reality it’s 38 to 40 hours a week.
“They are seeing more patients than ever before, which means GPs are working really hard and having to make very complex decisions, so to protect themselves they are reducing their working hours.”
The data, which was published by NHS Digital on Thursday, also shows that the total number of qualified permanent GPs in England has fallen from 27,912 in June 2017 to 26,859 in June 2022 – a drop of 4%, with a decrease of 0.6% in the most recent 12 months.
Working 'part-time' in general practice often means working what would normally be considered full-time, or longer - and will likely include many hours of paperwork on top of patient appointments— Professor Martin Marshall, Royal College of GPs
All figures are based on the number of full-time equivalent posts in the GP workforce, and do not include trainees or locums.
Professor Martin Marshall, chairman of the Royal College of GPs, said the drop in qualified full-time GP numbers was leading to a “chronically over-stretched and under-resourced general practice service”.
He added: “Working at this intensity is unsustainable and it’s unsafe for both patients and staff.
“An exhausted GP is not able to practise safely or deliver the high-quality care and services they are trained and want to deliver for patients.
“This is leading to GPs and other members of our teams burning out and having to evaluate their futures working in general practice, in some cases leaving the profession earlier than planned and in others reducing contracted working hours to make the job more sustainable.
“Yet working ‘part-time’ in general practice often means working what would normally be considered full-time, or longer – and will likely include many hours of paperwork on top of patient appointments.”
The college is calling for urgent action to develop and implement a recruitment and retention strategy to achieve and go beyond the Tory manifesto target of 6,000 more GPs by the end of the parliament.
Prof Marshall also said that funding for general practice needed to be returned to 11% of the total health spend and unnecessary bureaucracy reduced to free up GP time to care for patients.
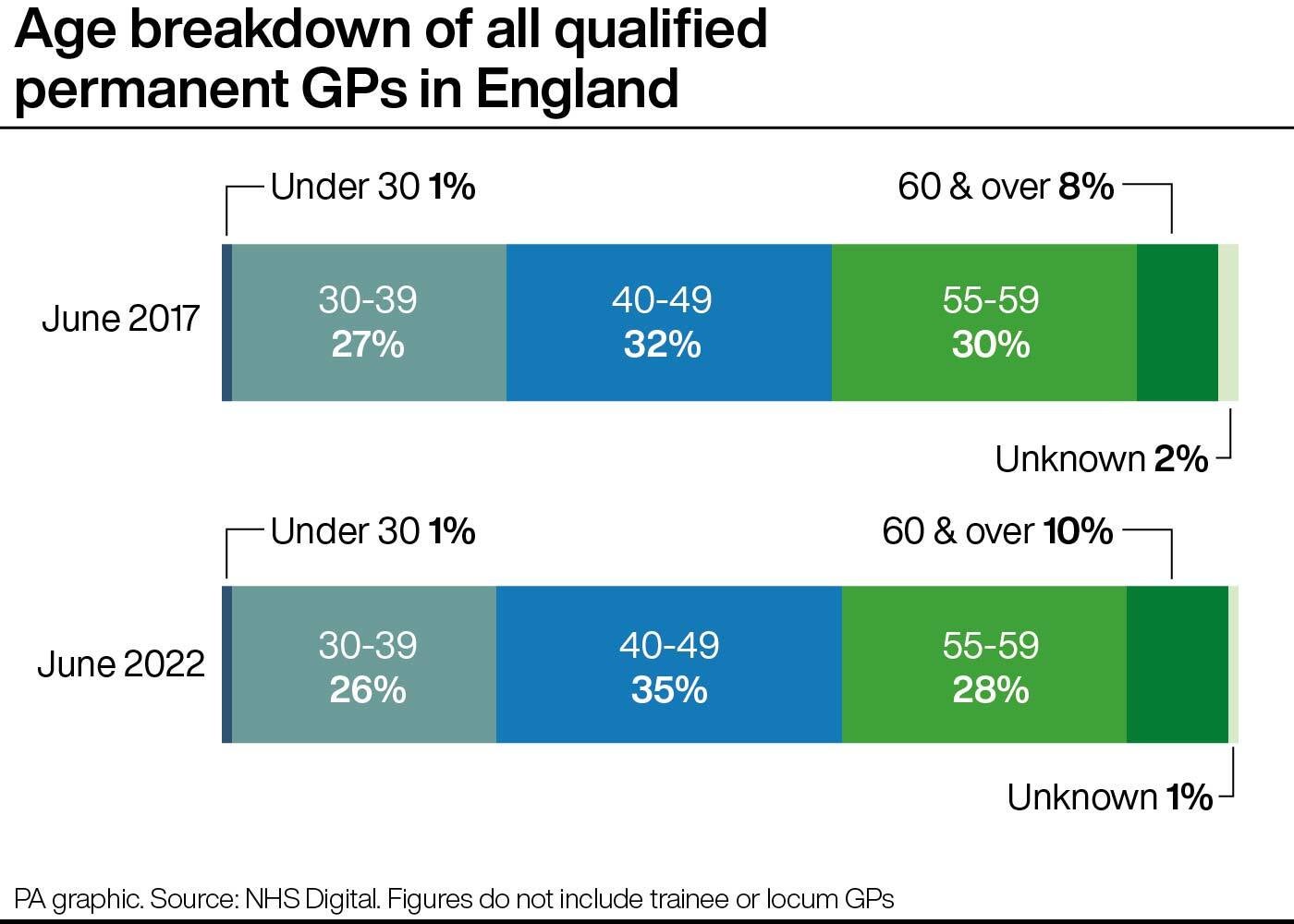
The new data also showed that the age characteristics of England’s GP workforce appear to be changing, with a growing proportion of doctors in their 40s or over 60.
In June 2022, GPs aged 40 to 49 accounted for 35% of all qualified permanent doctors, up from 32% in June 2017.
The proportion who were aged 60 and over rose from 8% to 10% over the same period.
But those aged 50 to 59 fell from 30% to 28%, while 30 to 39 year-olds dropped slightly from 27% to 26%.
Reasons for these long-term changes are not clear, but there have been reports of young doctors leaving the NHS to work abroad or older ones choosing to retire early.
The data comes amid mounting concerns about the number of GPs needed to meet the rising demand for appointments, which for much of 2022 has been higher than 12 months ago.
In June the Health Foundation think tank called for urgent action after it published a forecast showing a quarter of GP posts could be vacant across England in the next 10 years.
It found the current shortage of 4,200 full-time equivalent GPs in England is set to rise to 10,700 in 2030-31.
The Health Foundation analysis suggested the Government is unlikely to reach its target of hiring 6,000 additional GPs by 2023-24.
Meanwhile, the annual GP Patient Survey earlier this month revealed declining satisfaction with family doctors and that patients were putting off appointments because they find it too difficult.
Some 72% of patients in England said they had had a good experience of their GP practice early in 2022, down from 83% the previous year and 82% in 2020.
Some 55% of patients who needed an appointment said they had avoided making one in the last 12 months, up from 42% in 2021.
More than a quarter (27%) had not made an appointment because they found it too difficult, up from 11% in 2021.
And some 51% said they saw or spoke to someone at a time they wanted or sooner (down from 59%), while 53% who wanted a same-day appointment got one (down from 60%), and 56% said they had a good experience making an appointment (down from 71%).







