Chemotherapy has been used to fight cancer since the 1940s, radiotherapy was pioneered almost a century ago, and surgeons have been removing tumours in order to save lives for much longer. While these familiar-sounding treatments are still widely used today, they now look vastly different, are more successful and cause fewer side effects. So while one measure of progress in cancer research is that more people survive the disease – since the early 1970s, mortality rates for all cancers combined have decreased by around a fifth in the UK – another is that treatments can be less gruelling. The even more encouraging news is that, with the help of gifts left in wills to Cancer Research UK, all this progress is part of a trajectory still heading full-throttle towards an even greater understanding of the disease and, one day, the possibility of beating it.

A patient receives radiotherapy to the jaw, circa 1929 – the treatment was pioneered almost a century ago. Photograph: Barts Health Archives and Museums
Making treatments kinder
If you were diagnosed with breast cancer at the turn of the 20th century, doctors had to take drastic measures, cutting away the entire breast along with the underlying chest muscles and all the lymph nodes from the armpit. The recovery time from these radical mastectomies was long and some of the after-effects were for life, ranging from swollen arms and movement difficulties to poor body image, depression and anxiety. But through determined research and listening to patients more, by the 1960s there was enough evidence that a far less invasive lumpectomy had survival outcomes just as good as radical mastectomies for women with early stage breast cancer, while also minimising physical and psychological side effects.
Radiotherapy and chemotherapy are the other two main prongs in breast cancer treatment. As in many other types of cancer, radiotherapy is often used after surgery to kill any cancer cells that might remain in the area around where the tumour had been, but it comes with risks of causing permanent damage to healthy tissue, leaving scarring and hard areas of breast tissue. And it once meant 25 hospital visits over five weeks.


A cancerous tumour in the breast (circled), visible through a mammogram. Photograph: Science Photo Library
This was until two landmark studies, starting in the late 1990s and supported by Cancer Research UK, found that a smaller number of higher doses of radiotherapy were just as effective and minimised side effects, while reducing hospital visits for treatment from 25 to 15, spread over three weeks. In 2009, once the 10-year post-treatment outcome figures were in, the evidence changed the National Institute for Health and Care Excellence guidelines on radiotherapy for breast cancer. The efficacy of these developments along with others – more on which follows – is highlighted by the fact that the risk of breast cancer coming back within five years after treatment has dropped from around 10 in 100 people in the 1980s to between one and two in 100.
The next step is a study, still under way, called PRIMETIME, which aims to see if women who have only a small risk of their breast cancer returning need to have radiotherapy after surgery.
The age of bespoke medicine
Like our faces and fingerprints, every case of cancer is unique – and researchers have discovered many ways of reducing the negative impacts of treatments by tailoring them according to individual need. When Oliver, 60, was diagnosed with tonsil cancer in 2009, he had a tonsillectomy followed by chemotherapy, and then radiotherapy. This brings with it a risk of side effects arising from damage to healthy tissue, which in Oliver’s case would include a permanently dry mouth. But Oliver took the opportunity to take part in a key Cancer Research UK-funded clinical trial of a newer, more targeted form called intensity modulated radiotherapy (IMRT). In this treatment, the radiation beams vary in strength and intensity, allowing them to be shaped to target a precise area – either in the exact shape of a tumour if used to shrink it before operating or, as in Oliver’s case, the immediate area around where the tumour had been. “I feel fortunate to have been offered the chance to help medical research,” says Oliver, who recovered well.


Oliver, who recovered from tonsil cancer after taking part in a Cancer Research UK-funded clinical trial. Photograph: Jane Stockdale
The race to reduce complications when treating children with cancer reached a much needed milestone in 2022. The most common aggressive brain tumour affecting children is medulloblastoma, which grows in the cerebellum at the back of the brain. Every year in the UK, around 50 children face this diagnosis. Ongoing research has established four subtypes of medulloblastoma, which can help doctors develop better treatment plans. Around 70% of children survive medulloblastoma for five years or more, but recent findings by Cancer Research UK scientists, led by Prof Steve Clifford at Newcastle University, are paving the way for even more honed treatments.
“The sequencing tools available to us now allow us to see, in much greater detail, the driving forces behind the different types of medulloblastoma at the single-cell level,” says Clifford. Among their discoveries is that tumours in the subtypes with the highest survival rates contain genetically identical cancer cells, whereas the harder to treat tumour types have three or four different types of cancer cells. This gives them a better chance of evading treatment. The team also discovered a way to identify subtypes more easily, which could avoid the need to take multiple biopsies.

An MRI scan showing medulloblastoma, the most common aggressive brain tumour affecting children. Photograph: Science Photo Library
“We are now at the stage where we can clearly see what changes cause medulloblastoma to emerge in the first place, and the paths it can go down that determine how aggressive it is likely to be,” says Clifford. These crucial findings could lead to more effective treatments.
“No child should have to suffer a disability as a result of their cancer treatment,” says Prof Pam Kearns, previously director of the Cancer Research UK Clinical Trials Unit at the University of Birmingham, referring to the hearing loss experienced by more than 60% of young patients with hepatoblastoma – a type of childhood liver cancer. It’s a side effect of the most effective chemotherapy for this disease, but phase three clinical trials showed that the risk can be almost halved by taking a new drug, sodium thiosulphate, alongside it. The drug has now been approved by the Food and Drug Administration and European Medicines Agency for use in reducing chemotherapy-associated risk of hearing loss.
Meanwhile, yet more recent research has further honed treatment for breast cancer – the world’s most prevalent type of cancer. The drug Herceptin was developed in the 1980s after it was discovered that some breast cancers have large amounts of a protein called HER2, which makes the cancer cells grow and divide. Herceptin is a targeted cancer drug that works by attaching to HER2, stopping this process. A downside is that it can damage the heart. But in 2019, Cancer Research UK scientists published a paper showing that cutting the treatment time from a year to six months was still as effective at stopping cancer from returning, but it also reduced the risk of adverse effects of the drug.
A brighter future
While some treatments involve large innovations, others have benefited from small adjustments. Take the FOxTROT trial, which showed that starting chemotherapy six weeks before surgery for colon cancer, then continuing for 18 weeks after, cut the risk of the cancer returning within two years by 28%. Patients previously had surgery at the start of their treatment followed by 24 weeks of chemotherapy, however, the trial revealed that not only did chemo prior to surgery increase the chances of all cancer cells being killed, it also reduced the number of side effects from surgery, meaning patients were less likely to suffer infection or need further operations.
These results are particularly positive as, unlike many breakthroughs, this change is quick and costs little to implement, and can be rolled out worldwide. In many parts of the world cancer treatments can be prohibitively expensive, which is why the researchers behind the FOxTROT trial wanted to go in the opposite direction, testing a treatment that could be used on the widest possible group of patients. Doctors in countries around the world will be able to save many thousands of lives as a result of the trial, which was funded by Cancer Research UK.


Light micrograph of a section from a malignant pancreatic adenocarcinoma. Photograph: Science Photo Library
Pancreatic cancer is a common cancer in the UK – and one of the more difficult to treat – but the Institute of Cancer Research in London is testing a new targeted way of using radiotherapy that will minimise damage to surrounding healthy organs.

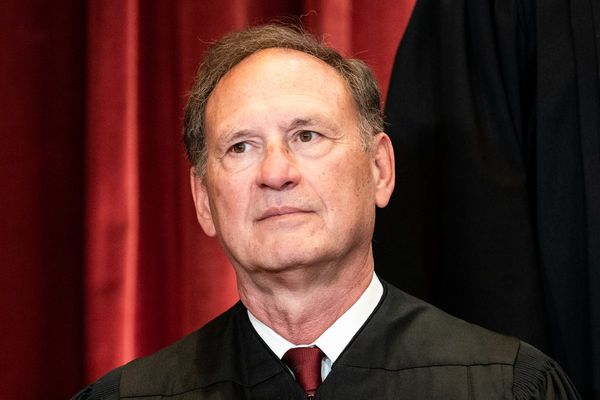
Prof Uwe Oelfke
The project is being led by Prof Uwe Oelfke, whose joint specialities in fundamental and medical physics mean he is well placed to drive the implementation of such medical treatment innovation. He and his team use a radiotherapy machine with a built-in MRI scanner that allows radiation oncologists to see inside the patients as they treat them, including the position of the tumour. Tumours will move during therapy due to breathing and can drift substantially during the days of a treatment course. As Oelfke says: “We don’t want to have to treat patients based on an image someone took a few days ago – we want to be able to treat what we can actually see in front of us at the time.”
While working towards setting up clinical trials for the machine, Oelfke is also busy establishing a research facility to investigate two potential new types of radiotherapy, called “micro-beam radiation therapy” and “Flash therapy”. These novel techniques require special equipment to produce either much smaller rays or deliver doses in much shorter time scales. For both techniques, preclinical trials have shown that they could eradicate tumours while sparing healthy tissue. “Ultimately, if we get this right,” says Oelfke of his work, “we’ll see better quality treatment and greater efficiency.” All part of the trajectory in cancer research that means ever better outcomes and improved quality of life for patients.
Funding the future
A pledge of a gift in your will could lead to investments in research that further change the outcomes for people affected by cancer, helping them live longer, better lives. These legacy gifts enable Cancer Research UK to commit to the large-scale, long-term research projects that yield the biggest breakthroughs. The advantage of pledging gifts in wills is that the income stream is guaranteed, enabling Cancer Research UK to invest in cutting-edge science with the potential to make the biggest difference to future generations in the UK and around the world.
Gifts in wills are vital to accelerating progress, and fund one-third of Cancer Research UK’s work, enabling lifesaving breakthroughs. To find out how you can help fund the next 50 years of progress by pledging a gift, visit cruk.org/giftsinwills