
Have you or a loved one ever needed surgery? Imagine what your life would be like if you couldn’t have it. Billions of people around the world lack access to surgery because equipment and general anaesthesia are too expensive or unsuitable in their region.
When we think about technological progress people tend to picture faster, shinier, more hi-tech upgrades of what we already have. But sometimes developers can have more impact by remodelling technology with cheaper and simpler versions.
Our group at the University of Leeds is developing surgical technology for low-to-middle income countries and our first project was a simplified surgical tool for performing laparoscopic – or keyhole – surgery in low-resource settings where it was not possible before.
Surgical technology has never been more advanced. The NHS is adopting robotic surgical systems, which give surgeons new levels of precision and skill to perform complex procedures for prostate, gynaecology and bowel surgery.
But while these advances are impressive, they highlight a stark inequality; an estimated 5 billion people (more than two-thirds of the global population) cannot afford surgery. And yet, surgery is the primary treatment for one-third of diseases. Of the 313 million procedures undertaken worldwide each year, only 6% are performed in the poorest countries, where more than one-third of the world’s population lives.
Why surgery is so hard to access
A shortage of trained surgeons, healthcare costs and cultural barriers (many people turn to traditional healers first) prevent access, but all too often there is not enough appropriate surgical equipment available. By that we mean technology that fits the resources and services available in the local healthcare setting and does so at a cost affordable to local patients.
The shortage of technology designed for low-resource regions is because biotech firms focus on the major commercial markets in the EU, US and China and are reluctant to undercut more expensive, profitable technologies.
The solution is not as simple as providing low-income countries with the same surgical technology used in high-income countries. Well-meaning donations of surgical equipment are often unused because they are too expensive to maintain. Communities struggle to source items such as air filters, cutting blades and CO₂ gas to make equipment work.
Research reveals 40-70% of medical devices in low-to-middle income countries are broken, unused or unfit for purpose.
What we did
We set out trying to develop new surgical equipment tailored to low and middle income countries, using “frugal innovation” as our guiding principle, meaning we were aiming to do more with less“. We also involved clinical staff throughout the process.
Our project helped surgeons practice vital keyhole surgery in remote areas of rural India. In laparoscopic surgery, the patient’s abdomen is inflated with CO₂ gas and the surgeon operates using long instruments which go through small incisions into the space created. The technique, pioneered in 1901 in Germany, revolutionised modern surgery, reducing their risk of infections and dramatically lowering the recovery time for patients.
Unfortunately, it requires general anaesthesia, and a reliable CO₂ supply, both of which are too expensive in low-resource regions. General anaesthesia must be administered by an anaesthetist. An alternative technique, gasless laparoscopy, uses a mechanical retractor to lift the abdomen and create space. This method doesn’t require CO₂ and allows the use of readily available spinal anaesthesia instead.
Spinal anaesthesia can be carried out by the operating surgeon, removing the need for a specialist anaesthetist. It means that patients in poorer countries can be given essential surgical treatments such as appendectomy, gall bladder removal, gynecological procedures. It also enables patients to return to work quickly, which is important because the longer patients are off work sick, the deeper they fall below the poverty line.
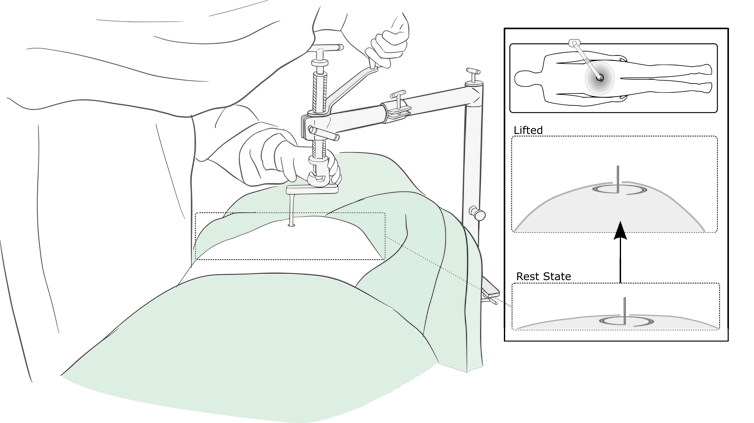
There is huge potential for gasless surgery but uptake has been limited because the retractors are bulky, hard to use and maintain and are expensive.
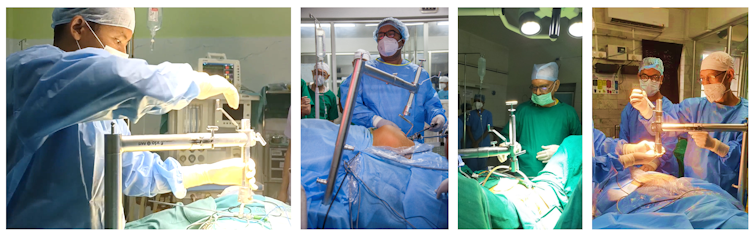
Our designers teamed with surgeons to create a modern retraction system. We worked together to understand their needs and develop better retractors through repeated testing. The result is "RAIS” (Retractor for Abdominal Insufflation-less Surgery) which is being produced by our commercial partner (Ortho Life Systems). It costs $980 (£802), about one-third of the price of the older retractors.
The response from our surgical partners has been encouraging. Dr Biju Islary, surgeon and expert in gasless laparoscopy at Crofts Memorial Christian Hospital, India, said: “I have been involved from the start … this is a very good device to use.”
It is being used in ten medical centres in rural Indian states and we are working to expand this to new areas in India and around the world.
A problem close to home
Even higher-income countries struggle with unequal access to surgical care. Postcode lotteries create disparity in availability of healthcare, in places such as the US or UK.
The UK’s Green Surgery Challenge has recently highlighted how frugal approaches could save the NHS money. For example, reusable instruments and surgical kit together with washable gowns and drapes, rather than single-use disposable items, are more environmentally friendly and cost effective.
Our aim is to form an international collaboration. We held the first International Congress for Innovation in Global Surgery in April 2022. There is a lot of scope for improvement in access to gasless surgery and we will work together to improve the other technology involved, including camera systems and monitoring devices.
Technology innovation has an important role to play in surgery. People get excited about the release of a new video game or smartphone – but what could be more incredible than saving a life? Few products have as great an impact on people’s lives as accessible medical equipment. It is time for technology developers to think outside the box and create surgical products for low and medium-income countries – a market of billions.
Pete Culmer receives funding from the UK Engineering and Science Research Council (EPSRC) and the UK National Institute of Health Research (NIHR). He is affiliated with the Institute of Mechanical Engineering (IMechE) Biomedical Engineering Division. The authors would like to acknowledge the research team whose dedication, passion and expertise have made this work possible, with thanks to everyone including: Association of Rural Surgeons of India and International Federation of Rural Surgeons, Anurag Mishra, Lovenish Bains and team at the Maulana Azad Medical College, New Delhi, India, Tim Beacon, Medical Aid International, Sundeep Singh Sawhney, Tamandeep Singh Kochhar and team at Ortho Life Systems, New Delhi, India; Richard Hall and Philippa Bridges at Pd-m International Ltd, Thirsk, UK; Millie Marriott Webb, Cheryl Harris and David Jayne at the University of Leeds, UK
Noel Aruparayil worked as a clinical research fellow funded by NIHR Global Health. He is on the Global Surgery Foundation committee for the Royal College of Surgeons of Edinburgh and sits on the advisory board for GASOC (Global Anaesthesia, Surgery and Obstetric Collaboration).
Jesudian Gnanaraj does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







