A former senior doctor from Newcastle 's blood transfusion centre said in 1983 there were "embarrassingly large" stocks of NHS blood factor concentrate products to treat haemophiliacs, but the RVI Haemophilia Centre director preferred to use commercially-made products.
In a letter from Dr Anne Collins, then-director of the Northern Regional Blood Transfusion Service (NRBTS), she asked Haemophilia Centre director Dr Peter Jones about using UK products rather than imported, saying: "We have an embarrassingly large supply of BPL Factor VIII in stock. How about it?"
Thousands of haemophiliacs who relied on the products were given Factor VIII contaminated with lethal viruses like HIV and Hepatitis C - more than 2,400 have died, and the number continues to increase.
Go here for the latest NHS news and breaking North East public health news
NHS patients were also given tainted blood transfusions.
As early as 1975, figures including Lord Owen - health secretary at the time - had set targets to achieve "self-sufficiency" in the UK's blood supply in order to lower the risk of transmitting viruses to patients.
However, throughout the 1980s imported commercial products were still used.
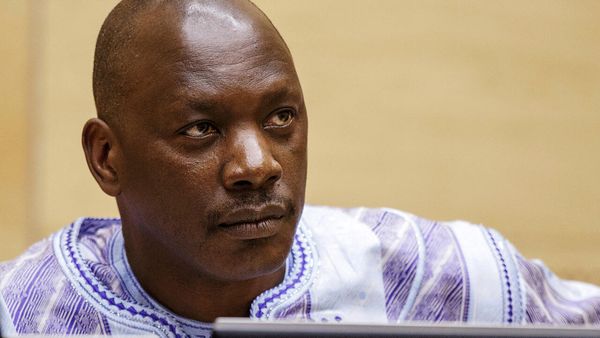
Giving evidence at the Infected Blood Inquiry, Dr Collins' successor Dr Huw Lloyd told the Inquiry's chair Sir Brian Langstaff how he had no direct knowledge as to why Dr Jones preferred to use commercial products.
However, he said: "The commercial Factor VIII was more easily soluble. In other words you could put the distilled water into the vial, and dissolve it much more quickly than you could the [UK] BPL product. So I actually experienced that.
"It is the case that that [UK] product, the BPL product, was less easy to use. It wasn't presented, if you like, in a nice package. It didn't come with with everything together."
Dr Lloyd was in the role from 1988 to 1995.
In a statement drafted by Dr Collins for legal action in 1990- and shown to the Inquiry - she wrote: ""It became apparent that there was a preference at the Haemophilia Centre for commercially produced Factor VIII blood product for the following reasons ..."
There would not have been enough UK-produced Factor VIII to match demand for the product, according to documents shown to the Inquiry - and Dr Lloyd agreed with this.
Dr Collins, the Inquiry heard, listed "solubility, allergic reactions, and a more attractive presentation of commercial Factor VIII".
In a previous written submission to the Inquiry, Dr Jones highlighted: "Any blood product, whether from volunteer or paid donor sources in the United Kingdom or abroad, carried the risk of viral transmission."
Dr Lloyd also spoke of how when he first began work at the NRBTS, conditions were "Dickensian".
Dr Lloyd also told the Inquiry how he felt medics could have done more to test blood products for Hepatitis C later in the decade, and spoke of how processes had to be changed in the late 1980s to ensure blood wasn't taken from "unsuitable donors".
The NRBTS moved into a purpose-built new building in 1985, but before that Dr Lloyd said: "Even then,it was a very old-fashioned set-up - a bit cobbled together with these sheds, huts, and the basement facility. The laboratory equipment was generally old, and laboratory benches...
"By today's standards, one would be horrified at the wooden benches and people actually brewing tea in a laboratory, which I recall.
"It was pretty outdated, even by the standards of the 1980s."
Dr Lloyd said clerks would be sat on "high stools at wooden benches with great big ledgers" and it "gave you that feel of a Dickensian office".
In around 1983, during his training Dr Lloyd also spent time in the Freeman Hospital's haematology department. At this time he had involvement investigating "clinical issues arising from transfusions".
He said: We saw some serious things. I do not recall anything that was related to non-A, non-B, for instance, but then I don't think people were looking as hard for it as they might.
Speaking of attitudes towards Hepatitis C as the 1980s developed, and how his own knowledge grew, Dr Lloyd said he felt medics should have been carrying out "ALT" blood tests to screen for the virus, which was then known as non-A, non-B hepatitis. He added: "Was I standing up there shouting from the rooftops, saying we should do it? No, I wasn't, and probably should have done more.
"But it took the UK seemed to have this attitude that this was not a serious disease, and we didn't need to do much about it."
As medical director of the NRBTS, Dr Lloyd said he brought in changes which meant blood donors were screened before donation, rather than screening their blood afterwards.
He said: "It highlights an issue that we tried to deal with later which was that we were taking donations from people where we weren't sure if their donations were going to be suitable for full use.
"We felt later - when we came to this issue - that we tried to change that round and say we shouldn't take a donation from someone unless we're sure that their donation is suitable for use."
Dr Lloyd - speaking via videolink from Canada where he now lives - will continue to give evidence on until Thursday February 10.
The Infected Blood Inquiry, which began in 2018, will continue to hear evidence from medics who worked in the field of blood transfusion and blood products throughout February and March - with further hearings on to continue through 2022.